
or Wry Neck
Moebius Syndrome
Goldenhar Syndrome
& variants
Occular Torticollis
Spastic Torticollis
Dystonic Torticollis
 |
The typical case is a baby with a slightly turned and tilted head. Most commonly, it isn't even noticed until two to three weeks of age. Sometimes a horizontal red line is seen at the base of the neck.
All that is is skin reddened from sweat trapped in the folded skin due to the constancy of the head being held to one side. Air, by drying the skin, makes that go away.
 |
Some of the more tilted and more rigid cases also have a lump on the neck muscle. It can feel hard. It isn't at all uncommon (sadly) to see parents with a sheaf of x-rays and studies trying to figure out the nature of this "tumor".
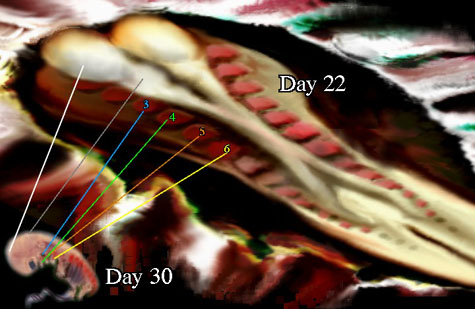
Torticollis begins with a fetal posture that has the neck tilted. If that way long enough, the muscle called the "SCM" shortens. Birth gives little time for gradual stretching and that SCM muscle may very well tear as the head goes through the twists of getting born. Because the muscle tears, the head is NOT tilted. The SCM muscle sheath fills with blood and presents a fairly normal contour (not a dent).
As the blood absorbs, scar tissue infiltrates the tear area and vessels come in to take away the debris - that's the swelling. Scar is nature's suture, it bridges defects then CONTRACTS. It pulls the torn ends back together. So at about two to three weeks we see the tilt for the first time, but it is really the second time as the initial tilt was out of view in the womb. The lump may be prominent or already gone.
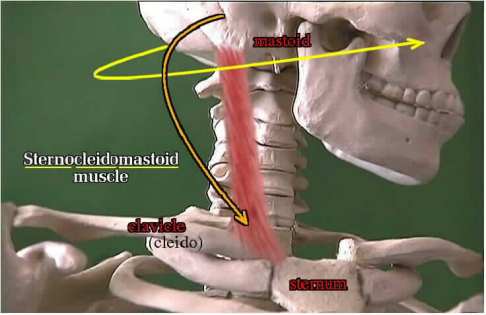
The "SCM" muscle is named by the bones it spans. Behind the ear is the mastoid bone (M). At the top of the chest is the sternum (S) or breast bone where it meets the clavicle or collar bone (C).
 |
So this muscle runs backward from the chest to behind the ear. When it shortens we see that combination posture of head turn to face the opposite side and head tilt toward the same side. Touch one ear to the shoulder and you perform this movement.
 |
Treatment is to gently and PERSISTENTLY stretch this one muscle to its optimum length . There are two ways. Grab the head and return to straight up. Then as stretch improves, tilt a bit the other way (the reverse turn and tilt). Often kids hate this head grabbing thing. If so, the other way is to cradle the baby and use the bed surface or soft rug as a resting surface for the opposite cheek as the body is lifted and body gently tilted a bit. The bed is a counter point. Be gentle, of course.
 |
RATHER THAN GRAB THE HEAD
 |
 |
Scar once contracted tends to return to contraction until it "matures". That is easily six months. In other words, if you succeed and then quit stretching before that you will see it back again. The more settled the scar (the more mature) the harder it is to stretch out. We really want to see this done with by age one. Many statistics show that strong contractures still present at age two will just not stretch. But statistics are not real science but rather batting averages. Look at the details. If the child is nearly two and tends to lean as described, but can be tilted the other way without too much ado, then it is more a matter of persisting than cutting.
Cutting? Oh, yes. If the muscle won't stretch, then like tight muscles elsewhere, we lengthen them. To avoid getting to this state of affairs do the stretching many times a day every single day. Sending a youngster off for somebody else to do it will fail. PT is good as a referee and teacher, not a substitute for home exercises.
 Sometimes we need to get nasty and just hold the head round the
clock. Body casts which included the head, called Minerva Casts, were used. The danger is if the child chokes, access can be impossible.
Sometimes we need to get nasty and just hold the head round the
clock. Body casts which included the head, called Minerva Casts, were used. The danger is if the child chokes, access can be impossible.
The alternative is a brace that does the same thing. Children who come to surgery usually also come to this brace. So do the exercises.
The key feature is a head tilt which feels stuck, limited by something. If the head feels supple and tilts a lot, or if the youngster often but not always tilts, be very suspicious that there may be an eye problem causing it. If the lateral muscle of the eye cannot fully control horizontal eyeball movement as used in convergence, then the youngster sees double. TTHHAATT IISS VVEERRYY AANNOOYYIINNGG. They quickly learn to substitute the oblique muscles of the eye by tilting the head so that the obliques are now in the horizontal plane. Casts and neck stretching do not treat Ocular Torticollis.
A child with neurologic spastic abnormalities may also have the SCM muscle involved. Spastic Torticollis is identified by the company it keeps. The same is true for Dystonic Torticollis. This last variant is seldom an issue right at birth as dystonia takes a while to evolve. However, there are dystonic torticollis complications of certain medications. If neck tilt posturing occurs while neurologic drugs are being taken, check with the neurologist.
 |
There are congenital syndromes which also tilt the head. The early embryo has gill clefts and gill arches (the tissue between the gill openings) which are very similar to other species. The development of right and left "somite"segments in the head and face area can get fouled. If so, we see patterns which correlate with the tissue distribution of certain gill segments. One such spectrum of anomaly is called the facio-auriculo-vertebral syndrome, or Goldenhar Syndrome. It is an under formation of the first and second gill arches. It can vary in degree from most subtle facial asymmetry to severe defects which include the face, ear, and vertebrae most visibly. The more profound involvement may also result in smaller or absent portions of jaw, ear or hearing, cleft lip/palate, heart septal defects and "patent ductus", hair distribution anomaly, and even basic neurologic problems of cognition. Limb and kidney anomalies may also be present.
The Moebius Syndrome has many similarities to the Goldenhar Syndrome in certain respects, but shares tongue and finger/limb defects. A small jaw may accompany webbed small or absent fingers (or toes). Cleft palate etc.., and cranial nerve palsies may be present. The teeth may be under formed as well. The nose is often broad. The lower eye lids may have problems.
In a similar embryologic relationship we have the Branchio-Oto-Renal Syndrome. Slight alterations of the outer ear as shape, size or presence of small pits are associated with kidney defects, branchial (gill) persistence as fistulas (tracts) and cysts, lacrimal duct defects, and hearing defects. Some folks call the small dimpled pits in the skin of the outer ear "kidney dimples" so as to emphasize where the next look ought to be directed.
There are other such syndromes.
Go: HOME EMBRYOLOGY GILLS


