Spondylolysis
Spondylolysthesis
This discussion deals with the surgical treatment of spondylolysthesis. This discussion assumes that conservative methods are either impossible or have failed. Conservative measures include braces, and types of bone stimulator devices that are worn externally.
 There is much confusion that stems from badly named conditions of the spine.
There is much confusion that stems from badly named conditions of the spine.
Distinct entities include
spondylolysis,
spondylolysthesis.
spondylosis,
spondylitis.
That people get these mixed up is no surprise.
Just for clarity: "spondyl" = "spinal"
The latter two above mentioned conditions are not being discussed in this section, as they are not pertinent to our discussion of spinal instability. Just pointing them out because of the similarity of their names. There is zero similarity in the nature of these two conditions to the first two conditions, spondylolysis, and spondylolysthesis.
spondylosis (say: spon- d'low-sis) is a name for a degenerative
osteoarthritis kind of spinal condition
spondylitis (say: spon-d'ly-dis) is an inflammation of the spine.
There are several kinds including overt infection
and rheumatic types.
"olysis" = "with lysis" = "with a hole" or "with a crack"
"olysthesis" = "with lysthesis" = "with slippage"
spondylolysis (say: spon- d'low- lye- sis)
spondylolysthesis (say: spon- d'low- lice- thee- sis)
 This is a side view of the spine just above the sacrum.
This is a side view of the spine just above the sacrum.
A break in the bone - not unlike a fracture - is seen in
the posterior part of the lowest lumbar vertebra.
 This is spondylolysis. A crack. Three years later, it came to include spondylolysthesis. That is,
movement or slippage.
This is spondylolysis. A crack. Three years later, it came to include spondylolysthesis. That is,
movement or slippage.
This is the difference.
The last lumbar vertebra is now seen sliding forward
on the sacrum below. The 'break' in the bone was not sufficiently stabilized by ligament or cartilage of sufficient strength to keep the vertebrae stacked properly one above the other. It can slide further.
 We will examine this condition, and why treatment varies.
We will examine this condition, and why treatment varies.
Spondylolysis and spondylolysthesis are related conditions. Again, 'Spondylo' means 'spine'. Lysis means to be divided, or more simply, a hole or fracture of sorts.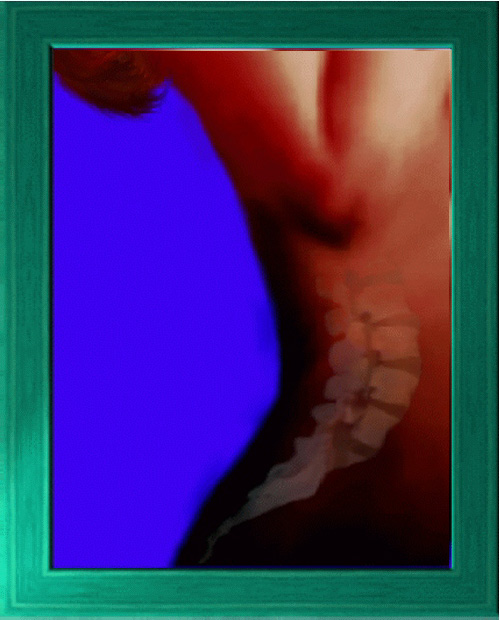
Vertebrae have two main regions,
1) the body which is the large drum shaped main column component in front of the spinal cord and 2) the complex
posterior elements, which roof the spinal cord and are in back, overlapping like shingles. The bumps you feel running down your back (the "spines") are a part of the posterior elements (spinous
processes). The overlapping feature gives the stacked column front to back stability, that is stability against horizontal shearing. Spondylolysis is a condition in which the back part of the
vertebra is not formed in one continuous piece of bone with the frontal, donut portion of the vertebra. It may be attached by cartilage, ligament, or scar. It may be or become totally detached.
Spondylolysis is a condition in which the back part of the
vertebra is not formed in one continuous piece of bone with the frontal, donut portion of the vertebra. It may be attached by cartilage, ligament, or scar. It may be or become totally detached.
For clarity of concept, some background info on bone formation. Sharks have full skeletons and spines with vertebrae but have no "bone" (the calcified SUBSTANCE). Their "bones" do not contain "bone". Got that? We don't spend much time floating. We calcify our skeletons for better weight bearing. Our bones are made of a material we call "bone".
When we are young, our lumbar spine individual vertebrae each start as one continuous bone made of cartilage, like a shark's, and later calcifies from several places at once. These spreading waves of calcification meet up and join (or occasionally not) at the area called the "pars". That's the spot where the x-ray sees a gap or hole because cartilage does not show on x-ray.
The lowermost vertebrae in the human spine, which are the most angled off the horizontal, are the ones most likely to crack when the formative process of replacement of cartilage by bone leaves this zone as cartilage. The sections of vertebrae involved in this cartilage-to-bone process are most at risk of coming apart where the carried weight is greatest and the shearing forces highest. That is, in the lowest two lumbar vertebrae (numbers 4 & 5 called L4 and L5).
Not only is spondylolysis a nasty name to say, but remember it is also often
misleading. In fact there may very well be no crack structurally; rather, the connection between the back and front in the vertebrae simply remains cartilaginous. About 5% of Americans have this variant and don't know it. One
group of Eskimo folks have a 40% incidence. It isn't a problem just because it shows on x-ray. It is just a trait - like blue eyes. So, 5% of our population has this. It is seldom much trouble beyond being yet another place
from which back ache can arise. It resides in the lower back. In that location the shape of the back is called 'lordosis', or incurved - the 'small of the back'.
So, 5% of our population has this. It is seldom much trouble beyond being yet another place
from which back ache can arise. It resides in the lower back. In that location the shape of the back is called 'lordosis', or incurved - the 'small of the back'.
Pain coming from this structure may refer to the hips or upper legs and be confused with sciatica. Unlike sciatica, it seldom reaches as low as the calves and never has weakness or sensation loss associated (as would nerve
pressure from a ruptured disc). If such additional symptoms are present, then an additional problem has also occurred
. One additional problem is that the cartilage segment gives way - cracks. It can also stretch. Or stretch then crack.
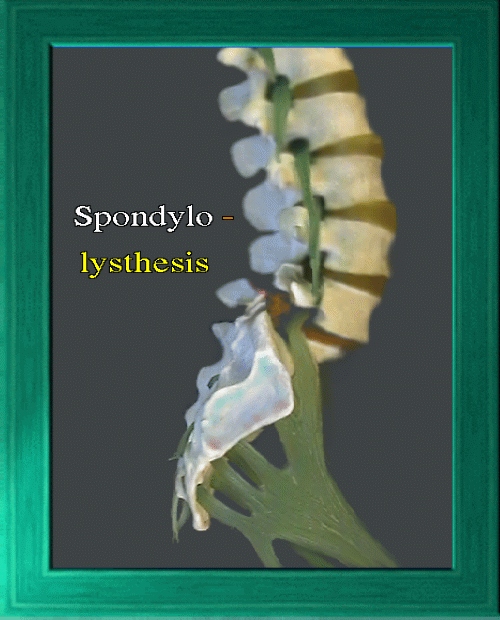 One may see a forward sliding of a vertebra relative to the one below it. This is usually due to 'pars defect'. The vertebral posterior elements overlap like shingles on a roof. A pars defect in the posterior element of a vertebra
means that this posterior element is split into two pieces. In this case, the stability inherent to overlapping vertebrae is lost. If the cartilage or ligament or scar residing in the pars defect is
not strong enough, then the upper vertebra can slip forward and even tilt if it goes far enough. The pars area of cartilage can also stretch, then heal, causing a limited but stable slip.
One may see a forward sliding of a vertebra relative to the one below it. This is usually due to 'pars defect'. The vertebral posterior elements overlap like shingles on a roof. A pars defect in the posterior element of a vertebra
means that this posterior element is split into two pieces. In this case, the stability inherent to overlapping vertebrae is lost. If the cartilage or ligament or scar residing in the pars defect is
not strong enough, then the upper vertebra can slip forward and even tilt if it goes far enough. The pars area of cartilage can also stretch, then heal, causing a limited but stable slip.
Slip is most common in the lowermost vertebrae because they are stacked at a
steeper angles. The more the lordosis (curve of the small of the back), the steeper the grade. Forward relative slippage is called 'lysthesis' - hence the
name spondylolysthesis. Even though the small of the back gets deeper and more 'lordotic' looking as slippage worsens, the actual slipping vertebrae may
be slipping forward relative to lower vertebrae, and they may begin to 'fall off' the front and tilt downward, which will be apparent on x-ray along the 'kyphotic' or frontal curve of the spine.
As the slippage increases, nerves may get either stretched or pinched. If slippage is very gradual, nerves may simply accommodate by elongating and there may be no symptoms at all despite very advanced displacements.
Therefore, symptoms of nerve origin are as much an indicator of rapidity of slippage as of degree. Sudden small slips may be more symptomatic than greater slips that took a long time getting there.
Such stretch symptoms can be profound or subtle. On the subtle side is hamstring 'tightness'. A person who was not particularly inflexible before, may become curiously tight in the hamstrings an unable to toe touch. Or, hamstrings can grip in spasm with pain and signs of nerve function loss. A very generalized compromise of multiple nerves of the low back is called 'cauda equina' syndrome. That is a bad one. It isn't just disabling from pain, it heralds dangerous function loss.
Treatment is based on presumed risk of progression derived from
1) that which has been witnessed in a series of x-rays,
2) the severity seen on x-ray,
3) kyphosis of the involved vertebrae (means it is falling unrestrained,
4) age.
An advanced slip - even asymptomatic - in a very young person is quite likely
to keep on going. In addition, such treatment as would be required to prevent slippage - an extensive brace plus restriction of all activities - may be simply too
oppressive to accept. Such "conservative" treatment is likely to fail, anyway in such a case.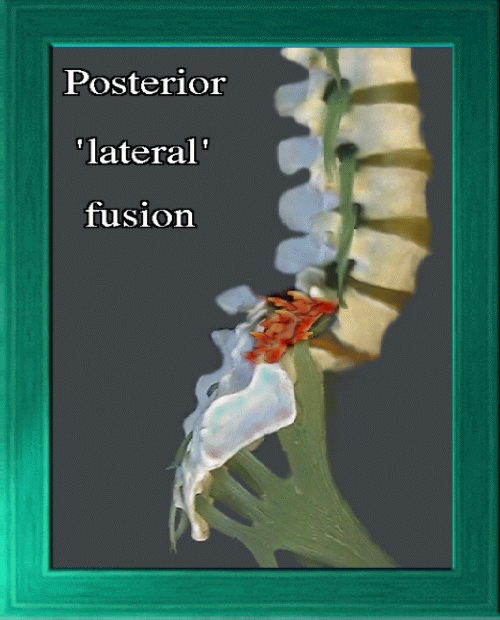
For these reasons, surgical stabilization may be opted for when conservative
treatment is oppressive, unlikely to work, or if neurologic findings or indicators of rapidity of slippage are present.
The old 'standby' operation is
postero-lateral spinal fusion
of the involved area. The intent is to fuse the vertebrae included in the surgery into a single, solid boney unit.This surgery can be done with or without metal stabilizing instrumentation.
Instrumented or not, spinal fusion surgery always incorporates bone grafting - the inserting of bone or bone-inducing substance into the gaps between vertebrae. In the very advanced slips
, metal instrumentation reduces the scope of the surgery (how many vertebrae you need to include), reduces the convalescence time, and increases the
successful surgical fusion rate. When the slippage is advanced, if metal is not used, this then requires including more vertebrae to get greater mechanical
advantage and sufficient bone mass to be sufficiently strong. Bone grafting, by itself, only places bone chips into the gaps, and since "fusion" (healing together
of the pieces into one continuous bone) takes many months, additional slippage can advance during the healing period post surgery (much less true with metal instrumented surgery).
 When such additional slippage risk is high, immediate surgical stability may be added by
metal devices of various types. These are used along with bone grafting - not instead of bone grafting. Fusion with bone graft is always used along with any metal placed. Metal is considered an internal brace, a temporary
treatment, until bone heals the parts together.
When such additional slippage risk is high, immediate surgical stability may be added by
metal devices of various types. These are used along with bone grafting - not instead of bone grafting. Fusion with bone graft is always used along with any metal placed. Metal is considered an internal brace, a temporary
treatment, until bone heals the parts together.
It is likewise true that steep advanced slips are as unstable for metal devices as for fusion alone. In advanced cases, additional vertebrae must be included to gain sufficient holding strength and provide sufficient bone graft mass to eventually take over. The downside to adding additional vertebrae to the fusion is additional low back stiffness.
This is the mobile area of the back. Fusing more vertebrae in the low back is associated with stiffer movement. Leaving additional vertebrae free (conservative fusion) is associated with a higher incidence of surgical failure - a very high percentage - in cases when slippage is advanced, the patient is young, or neurologic findings are prominent (Oh, by the way, fusions fail to work regularly in smokers. Smoking poisons bone fusion.).
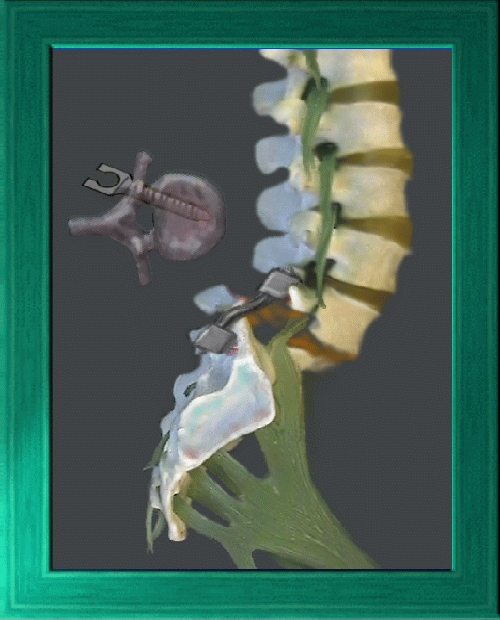
 To deal with the above problems, 'anterior' fusion is done (in addition to posterior fusion
or instead of it- as need demands). The larger and better kind of bone in the frontal vertebral bodies makes that a better place to gain not only fusion but immediate stability.
To deal with the above problems, 'anterior' fusion is done (in addition to posterior fusion
or instead of it- as need demands). The larger and better kind of bone in the frontal vertebral bodies makes that a better place to gain not only fusion but immediate stability.
Extensive removal of the spongy spacer disc between vertebrae is performed, and then
anterior bone grafts are put in place. These grafts are of two kinds, the fast-healing flakey bone chips, and the motion-stabilizing large keystone-like insert called a 'rabbit', which is geometrically shaped and inserted
into the inter-vertebral space to give stability and prevent further slippage.
The advantage of faster fusion, faster stability, better post fusion flexibility and
less post op pain make this a seductive choice. The 'anterior' operation may be performed entering from the side.
The problem with anterior fusion is that many orthopedists are not at home in this location and opt to stick to territory familiar to them. Certain older "anterior" operations were rather zealous at undoing the pathology and did have a track record of a certain percentage of patients with foot drop. That has been avoided in more recent practice with improvements in surgical methods and tools.
It is important to know that surgery is not immediate in its effect but requires healing time to be effective. 'Fusion' is the joining together of bone chips into a single unit - like bone healing. It not only takes time, but it takes protection. Extremes of motion during healing can thwart the bonding of these chunks into a cohesive single unit. Strength of that bond also is a variable. A thin bone bridge can stretch or break. Advanced slippage creates long distances for bone healing and orients the direction of the bond badly for effectiveness.


