
Severe neurologic or muscular diseases can deform to awesome degrees. We need to say
a few things about these cases as the peculiarities of treatment do NOT follow from the generalities of scoliosis as it affects otherwise healthy persons.
Progression is faster and younger. We do see cases of 90o curves in 4 year old children. Even when surgery is clearly in order, the problem of growth continues - too much or too little.
Too little: If the full length of spine is fused in a 4 year old, then spine height is arrested at that size. Fusion stops longitudinal growth of the fused region. An adult body size with a small child sitting height might be all that can be opted for. However, we do seek vigorously to deter surgery to allow height to mature. That is only wise as long as the curve is not simply folding. There may be temporizing methods which include partial fusion or instrumentation without fusion etc.. Bracing continues even when such treatments are used as growth is not done with its nastiness.
Too much: Even when the spine is fused, if the full circumference of the spine is not included, growth outward goes on. It can spin the spine like a helix around metal implants. Growth is very powerful in the very young.
In cases where reasonable maturity of length has taken place but stoppage of growth is not seen and the definitive surgery is needed, stopping the growth of the most troublesome section(s) will prevent the late post surgical deformation and also allow far better correction at the outset.
 |
Above are two similar cases of modestly severe curve progression that have not yet gotten to unwieldy degrees of curvature. They could easily be significantly improved with posterior surgery alone. However, virtually certainly additional deformation will resume because so much growth is still ahead. We can tell that from a whole bunch of fairly reliable findings. By attacking the curve front and back at the worst part, excellent corrections are achieved. The straighter you get the spine the less it tends to redeform when held.
 The spine, seen from the front is a series of
Vertebral bone drums separated by bulging discs. At the left is an x-ray for
orientation (*) marking where a nibbling tool (silver) removes the disc. This is NOT like a disc removal for "ruptured" disks. To remove a disc rupture is akin to wiping the dangling snot from a
child's nose. This is akin to removing the entire nose. The disc and its supporting container and ligaments are excised right up to the vertebra's bone - creating a gap
. That gap will bridge with bone (graft to promote that is placed into the space). However, the gap can be closed and provides a place to correct the deformity without
stretching. The correction by collapsing rather than by pulling from the ends (elongation) is what really makes anterior surgery so much more powerful - less traction on the spinal cord.
The spine, seen from the front is a series of
Vertebral bone drums separated by bulging discs. At the left is an x-ray for
orientation (*) marking where a nibbling tool (silver) removes the disc. This is NOT like a disc removal for "ruptured" disks. To remove a disc rupture is akin to wiping the dangling snot from a
child's nose. This is akin to removing the entire nose. The disc and its supporting container and ligaments are excised right up to the vertebra's bone - creating a gap
. That gap will bridge with bone (graft to promote that is placed into the space). However, the gap can be closed and provides a place to correct the deformity without
stretching. The correction by collapsing rather than by pulling from the ends (elongation) is what really makes anterior surgery so much more powerful - less traction on the spinal cord.
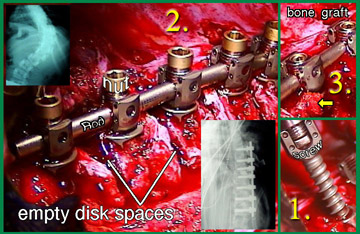
On the right:
1. A screw being placed across the vertebra body (first measured and the path tapped). A washer-like
staple protects the entry point.
2. Rod placed into the screw ends gets secured with bolt-like caps. Those caps have a handling protrusion. Note how the empty disc spaces are closed down with a bit of grafting
material smashed within.
3. The caps protrusions are removed after the rod is spun, shaped, and screws positioned optimally. The small arrow shows some of the grafting material oozing out as the space is pressed shut.
The inset x-rays show the before and after spinal shapes.
In some parts of the world, spinal tuberculosis is not a historical curiosity. Extreme deformity can occur all at one abrupt level as the bone of the spine, eroded away, just collapses. Paralysis might occur as an end result rather than as a cause.
 |
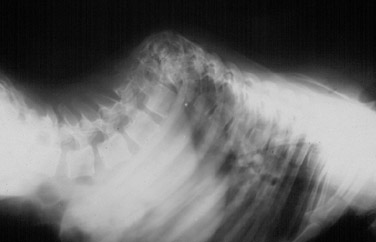 |
Obviously, direct treatment of the infection is important. Stabilization of the spine is made difficult by bone erosion precisely where bone healing and stability is most needed. Dr. Luque, in Mexico, developed the sublaminar wiring methods for precisely this problem. Massive strength of the metal implant is important for such circumstances.
Muscular Dystrophy (Duchenne's) is a special case. It has been determined by rather good statistical methods that no treatment other than surgery works if scoliosis occurs. Worse, conservative methods delay the surgery, but physical ability to withstand surgery drops off with time. Thus, conservative treatment greatly increases anesthetic catastrophe by shifting the stresses of surgery to a time when they cannot be endured.
Collagen Disorders are also of special interest. Typically, absent neuromuscular disorders , a scoliosis at or below 30o will not likely progress once growth is completed. For a child or adolescent Marfan's syndrome, this isn't true. Scoliosis, even in smaller degrees of curvature, might not stabilize with completion of growth.
Polio is still seen. One of the problems is that the bone MIGHT be thinned and less suitable to certain kinds of fixation. Also, persons with polio walk with amazing little muscle power in either leg (sensory mechanisms are intact and allow exquisite compensatory mechanisms of propulsion). Unfortunately, for spinal surgery, many of the tricks used by folks with polio are torso flipping or thrusting moves and pelvis wobbles are also common. The dual issues are 1) increased stresses on spinal instrumentation and 2) potential loss of flexibility that is being used as a substitute movement mechanism. Careful consideration of the benefits of "better correction" need to be weighed against less correction but more preservation of movement. It is a tough call at best.
This eight year old girl has the body size of about six years. Her seizure disorder was very difficult to control despite many medications and a vagal nerve stimulator (the large round device implanted in the chest area- our right, her left). Many pneumonias further debilitated her with less and less ability to resolve them. This is despite an implanted feeding tube and anti reflux surgery that had been performed. She had serious bone wasting and was apt to break bones at minimal stress. Bone enhancing dietary and medical therapies including diphosphonates were used to somewhat offset her bone wasting. Note the small round device just below her right (our left) collar bone. That is an implanted emergency venous line required by her many medical collapses and difficult vein access.
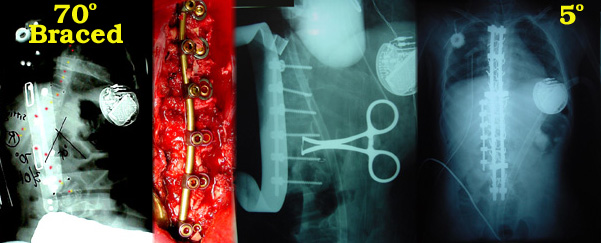 |
At the time of the x-ray on the left, despite two aggressive braces (a daytime brace designed to be optimum when sitting and a night time designed for recumbent posture), control was lost. A braced curve now = 70o. This was due to loss of seizure control with severe asymmetry of muscle tone from overt and sub clinical seizure activity and that was in turn stimulated by an intractable pneumonia which was confounding seizure treatment. She was clearly in need of stopping further spinal curvature which compromised lung expansion. Yet surgery was not safe in this state.
Botox paraspinal injections allowed the curve to relax and to be pushed to 30o. With that her chest expansion improved and the pneumonia was cleared. In turn, better respiratory function allowing respiratory acid base balance was followed by seizure stabilization.
This island of health was taken advantage of. The second image (red + bar) is a miniature fixation device which was used on her tiny bones to tame the seriously kinked segment of spine from the front. The next image (x-ray with operative tools in place) shows the substantial correction of that bad short segment. However, her bones were very soft and other curvature likely, and so the posterior more extensive stabilizing dual rod hook-hybrid was also placed. She has done well
AFRAID to INCLUDE THIS but ...
SPML of SPINE ?
...I must. What if the scoliosis is so bad that a very big spinal fusion is absolutely
required to save life itself? That is, in paralytic scoliosis, sometimes the case.
Yes it is. Botox? But what if the youngster is so ill or so small or has other ongoing medical problems that any corrective fusion will probably not be survived, but the Botox cannot undo actual stiff curvature that has quickly accumulated?
Well we have used SPML (seriously). We gave it a different name in our scoliosis study as it was a very limited form and not clearly just myofascia - some ligamentous stuff as well. So we called it apical release. Small number of cases but it did work.
We have come a long way and now see that in severe curves in very sickly kids the scope of scoliosis can be reduced by the SPML approach preemptively rather than as last step before eulogy.
In this extended use, the SPML is more typical of SPML in general and not just limited to apical stiffness. It seeks out curve causal contraction as well as contracture.
One case really stands out as several of our nation's biggest teaching spinal centers considered it inoperable. Look at this x-ray taken shortly before 'malignant progression' happened. Best bracing and seating attempts did no better than this.
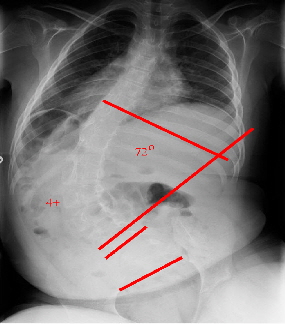 |
A medical ethics committee with trustees was convened and considered the case too far gone & at high 90's inoperable. That conclusion activated our IRB protocol (for hopeless & can't make it worse).
SPML, which took just a few minutes, attained a correction (to 10 degrees). Blood loss = less than one ml. Post op, cardiodynamics were much improved. Of course bracing is needed to hold correction (which was impossible before SPML).
 |
We are over a year and still holding.
We have other cases with similar results. The question is whether the SPML should be done earlier and not when impending death triggers an experimental protocol. As the series is published and reviewed we are coming off IRB as regards near death. We are not sure how best to proceed in preemptive use so as to allow statistical review of whether it adds something useful or just makes more work.


