
|
Mini-Thoracotomy
|
There has been recent discussion of thoracoscopic spinal surgery as, perhaps, a better surgery for scoliosis. It has, indeed, been stimulatory in the direction of innovation and, in some hands, refined for certain troublesome disorders. For example, Dr. Alvin Crawford (in Cincinnati), shared his refinements for very difficult cases of neurofibromatosis. Dr. Crawford is a class act and thoracoscopic methods as performed by him for the indications which he has furthered are hard to fault, especially when you see what he has been able to accomplish.
But then, some folks gloss over details. We hear of thoracoscopic surgery as a teeny weeny itty bitty replacement for the "old" and by inference "antiquated posterior surgery. It is also put forward as a replacement for the also "old" chest techniques with their chest gashes portrayed ala Hollywood B movie.
Itty bitty sounds good, huh? Mmmmm.
The problem is that precise indication and defined scope of application gets lost to what seems like promotion.
We have seen complication rates of as high as 100% from advocates of this method (requiring not so teensy weeny reoperation by other methods). Now, that isn't happening everywhere, but it is happening. This web site is about savvy. Let's tell what is and what isn't.
 The itty bitty thing. Thoracoscopic "portals" are not pin
holes and not just one one hole in one spot. Typically 3 to 4 (more often 4) portals are used. A portal is a tube about
the girth of a narrow garden hose.
The itty bitty thing. Thoracoscopic "portals" are not pin
holes and not just one one hole in one spot. Typically 3 to 4 (more often 4) portals are used. A portal is a tube about
the girth of a narrow garden hose.
Here we see post op portal wounds, in a male. There are three in this case as the curve was short (not many
vertebrae). The red circle indicates an area where such a scar could leave a pucker in breast tissue. Anterior and proximal placement of portals can significantly alter breast contours.
During surgery, portals (which look not too unlike funnels used to change car oil) stretch these incisions. Surgical tools are passed through the funnels. They are swapped
on the fly. That is, work is done with long tools through one portal while the thoracoscope, held by an assistant, videos through one of the others. Then the scope
and the operating portal paths are traded or both move to yet other portals.
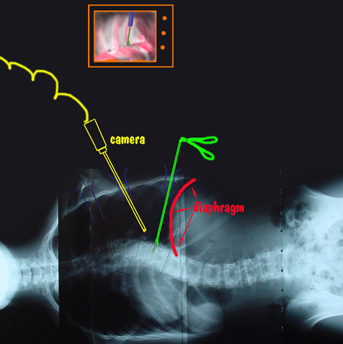 Multiple portals are needed because the long skinny surgical tools work
straight ahead and don't follow the curve of the spine very well. The line of sight as seen by the operating team on a television monitor (captured on
TV through the thoracoscope) is not the same as the actual path being used by the surgeon with those long skinny operating tools.
Multiple portals are needed because the long skinny surgical tools work
straight ahead and don't follow the curve of the spine very well. The line of sight as seen by the operating team on a television monitor (captured on
TV through the thoracoscope) is not the same as the actual path being used by the surgeon with those long skinny operating tools.
Three dimensional surgery is being controlled with two dimensional televised oblique vision. The far side of things can't be seen nor felt. X-ray is liberally used to orient depth of tools and figure actual orientation.
If the spinal curve extends much below the diaphragm, then it is out of reach of the thoracoscopic method.
A Case:
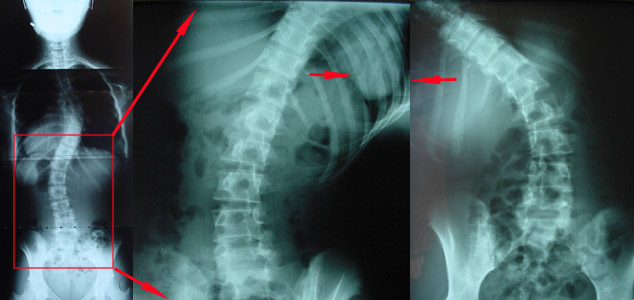 |
This one was not one of ours (not initially). It was the ideal thoracoscopic situation, though. The degree of curvature (in the chest above the red box) was not at an extreme. The curve was reachable from within the chest zone (that is, can be reached end to end within the cavity which houses the lung once that lung is deflated).
The red square points out the secondary curve, below, which on "bend films" behaved as supple. These x-rays were taken with the patient bending to one side then toward the other.
Had this lower secondary curve been stiff, then straightening out the upper curve alone would be a nightmare leaving the patient bent over to one side. A spine in the shape of an "S" is far better than one in the shape of a "7". That is, you ought not correct a "zig" more than the "zag" can spontaneously correct, or else the end result is a severe upper lean over a curved base.
If fusion fails, metal fails. Period.
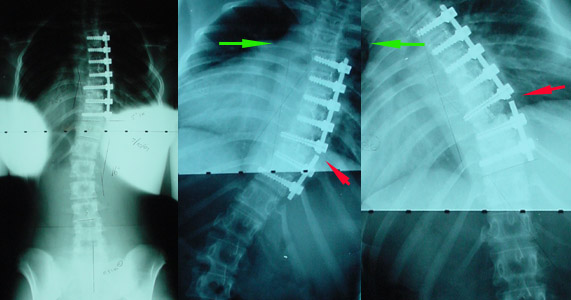 |
On the left is the post op thoracoscopic result. Looks pretty good. Then, later, the curve clinically worsened. X-rays revealed that the fusion failed and the metal broke. To remove such metal and explore the failed fusion site required a wide access using a full thoracotomy.
 The long U shaped horizontal full thoracotomy incision is seen. One portal scar was excised by the path of this incision. Another is covered by the red gown.
The long U shaped horizontal full thoracotomy incision is seen. One portal scar was excised by the path of this incision. Another is covered by the red gown.
The disc area where fusion had failed, when seen under direct vision, was observed to be only partially excised - though it probably originally on the TV monitor looked like an "extensive" resection, as that was how it was described.
Other complications of thoracoscopy have been reported. They have included life threatening vena cava laceration and gross surgical contamination stemming from esophageal laceration. There may be a high usage of x-ray, which is worrisome. Thoracoscopic tools do not allow for subtle rod re-contouring. There are very high rod end pull out forces which lead to a high metal to bone failure rate (screws yank out).
Mini-thoracotomy is, we think, a good alternative for the same purpose. It does not compromise the nature of surgery nor dictate instrumentation. It is well away from the breast area as it utilizes a single small posterior (not a typo) skin incision to do the anterior fusion and instrumentation.
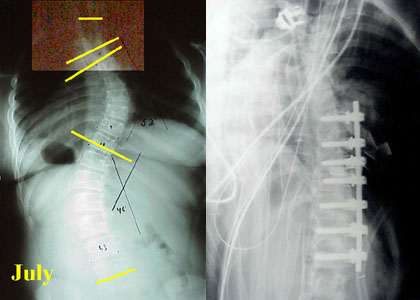 |
The above is an example of what is possible. Note that the curve is contained within the "chest" region. That is, with the lung deflated, the chest cavity gives access to the full extent of the curve.
In this case, other x-rays were taken bending first toward the left then toward the right. They showed that the lower curve was highly flexible and might behave if the chest portion were straightened. There always has to be an option, with all methods, to also do the back side of the spine if the anatomy happens to not be well behaved.
The front of the spine from the back? How is this done?
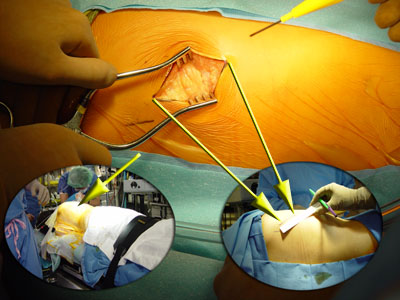 The oval inset images orient and size the incision (which is about 2 1/2 inches).
The oval inset images orient and size the incision (which is about 2 1/2 inches).
Lower left: Chest entry is actually posterior - just below the "posterior axillary line"
( the back edge of the arm pit).
This scar heals narrow and is hard to see.
The skin is moved headward or tailward several rib levels to access higher and lower sections of the spine.
 Skin stretches. Direct access to the spine allows normal surgical methods, optimum surgical instruments, a variety of implants as well as finger
palpation and visual protection of organs.
Skin stretches. Direct access to the spine allows normal surgical methods, optimum surgical instruments, a variety of implants as well as finger
palpation and visual protection of organs.
Unencumbered direct two eyeball 3D visibility and direct finger tip feel allow a high degree of precision. An assisting thoracoscope can be added for the assistants. It is no longer needed as newer corner instruments, for that purpose, utilize the main incision. Skin markings (in purple) map out the other levels which this one incision will be moved to access.
This exposure technique has now been further advanced to take full advantage of its better access by employing our newer nonparallel metal constructs which resist end pull out. That is another reason for this choice over thoracoscopy.
This method of surgery was recently presented at the North American Spinal Surgery Association meeting in NYC in April of 2002 in association with the Brazilian counterpart and the Iberian South American Spinal Surgery Association. It was was first presented in a spinal surgical forum in Brazil (a year prior).


