Muscle transfers
There are impressive things in medicine. Heart and kidney transplants breathe life into seemingly hopeless situations. Antibiotics save lives that would have been doomed. So many wonders, yet, they share one commonality, they keep the status quo. They maintain, protect, or extend.
In our field, we also have an additional directive, to build what never was but ought to have been. There is no greater satisfaction in medicine than to carve function out of debility. Weighed against this is the fear of making a bad case worse. With this perspective, we discuss muscle transfers.
In the movie Star Trek "The Wrath of Kahn", James T. Kirk was charged with having changed the computer programming of a Star Fleet combat test simulation because it was designed to be impossible and he didn't like losing. With muscle transfers, we do likewise. There is no solace in failing when the odds seem unbeatable if that loss leaves a function-less child behind. The proper thing to do is to cheat.
But how can we cheat? "Diagnosis" is nearly useless in this arena. Descriptions of what is wrong with the child, in Latin, Greek, or ICD9 code, achieves nothing useful. The wrongness is usually overt, obvious, and easily described. What we do need, is to inventory what IS working. We need a list of what is right, what is still working, and what isn't but can be made to work. We need to know what we have, and what we can SPARE. "We'll make use of this here, so let's put this there. We can give this up, so let's use it for that instead." That is the essence, the rest is just details and knowing stuff - stretch lengths, power ratios, blood supply and nerve attachments - doctor stuff.
The key to moving muscles around is knowing if the patient has the wherewithal to actually use what is moved in the way desired. We assume that the patient does if that patient has "the moves" and if there is a sensory mechanism in place. The key to repositioning muscle is not the cutting and sewing, but the knowing - What muscle can do what and will it know to do it? Invariably, the predictive answer is not found in muscle testing, but in sensory testing. Very important is a child's quick response to subtle unexpected prods. We learn much from observing play and wrestling. Watch a child try to evade an attacking swerving tickle hand - what movements, actions does the child seem to be trying, what appears to be intact?
Muscle transfers come in two types:
1) Take a muscle and give it an entirely new function, put it somewhere else.
2) Take a muscle that has several functions and remove some of the less needed
actions leaving it nearby where it was.
Recession:
Last first. When the brain's motion-generating
computer is damaged, complex information feeding back from muscles that have multiple actions - is - well - confusing. So many cross references need to be made. So many reflex interactions occur. Things happen too fast for it.
No time. Thus, no use.
By taking a "bad" muscle which is naturally set up to perform several tasks and, instead, giving it a single linear action, rather than its clever multi-use capability, not only do we gain a dedicated action, we also gain sensory input. Why? Simple action provides simple feedback that demands no cross checks. If a muscle only does one thing, feedback only reflects one thing. Simplified feedback is the cheat we need to get around the complex programming impasse. Simple feedback allows surer interpretation and faster response. Speed is everything. Motions that take a pause to figure out then perform are close to useless. We fall at 32 feet per second squared. We have to beat the gravity of the situation.
It isn't an official term, but in reconstruction, a transfer that removes actions in favor of just one of the original functions is called a "recession" because of the typical way they are handled. Usually recessions recess, move a muscle attachment back from across a joint, neutralizing action on that joint.
Example: The rectus femoris is normally attached to the patella to be a knee extensor along with three other muscles doing likewise. Collectively the four are called the quadriceps (in the sense that four singers who share a single stage are called the Four Tops). They act as a unit, yet have discrete capabilities.
But what if one of those singers was also a part time auctioneer? That might screw things up. Well the rectus femoris also attaches at its other end above the hip on the pelvis. Very clever tone adjustments allow that muscle to act on behalf of the knee and the hip in one combined, ever-adjusting tension and range decision, which works as long as there is good feed back from multiple sources and fast computation.
If hip auction-calling stifles knee singing, then best drop the auction-calling activity. There are plenty of hip callers, we can spare the rectus femoris there, where it is really just a back up. By recessing that muscle off the pelvis to the femur, motion of the hip is no longer felt in that muscle nor reacted to by that muscle. Likewise, sensory information reported back from that muscle can only mean knee, and in a direct linear way
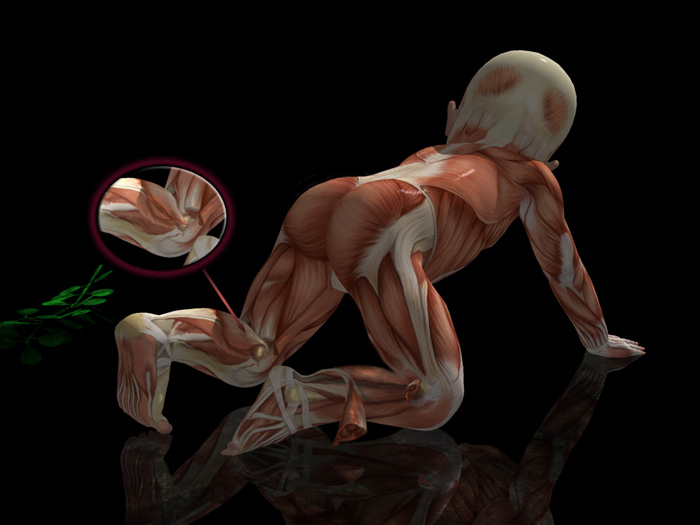 |
Muscles are shown cut away for visibility (we don't do that in surgery!). In the right leg, removing the lateral gastrocnemius shows that the really big unit of the calf muscle is deep - the soleus. It attaches to the tibia. The medial & lateral gastrocnemius muscles share the Achilles tendon with the soleus. Together they are also called the triceps surae. The medial & lateral heads attach above the knee to the femur.
Look at the left leg where the hamstring portions were removed for your benefit. It shows the medial gastrocnemius looping over the femur medial condyle like a string on a spool. When the knee extends this bit gets wrapped and tension develops. If overly reflexive this tug triggers a back reaction and fires the gastrocnemius in part or totally. If the muscle group is NOT short nor tight but merely prefires due to an extending knee (causing a reactive toe walk) then the inset show that moving the attachment off the spool on to the side at a neutral point will remove that reflex and not lengthen at all. That's a recession. Sometimes recessions gain length but often they can be done to remove spastic reactivity.
.
Here's another example. This fellow stumbles because his foot hangs down when he runs or if he tires. He does well with a brace, but wants that brace gone. It isn't cool. He also gets corns on the tops of
his toes, especially the great toe. Somebody told him to have the tendons snipped and the corns would go away. True enough. But, look closer (with the aid of high speed ceiling and side wall video
cameras). His ankle up-pulling muscle is weak, but the toe muscles are taking over, especially the great toe extensor. Before those muscles (which live in the shin area connected to the toes by long
tendons) can raise the foot, the toes have to hit the end of their range. That is why they press against the top of the shoe toe box and get corns. You can see the tendons prominent from the ceiling view.
If those tendons were attached to the metatarsals en route to the toes, then they would stop causing corns and have better mechanical advantage on the foot. This is a recession. Give up
the ability to raise the toes (only with these muscles, there is a second set) and gain the ability to raise the ankle and give up the brace. Crossing fewer joints, the muscle feed back would be
better linked to ankle position and give a better control ability for faster activities.
Transfer:
Give a muscle a different job, altogether? In a stroke patient who exhibits stiff knee walking, the far end of the rectus femoris (one of the four from the quadriceps muscle unit), near the
knee, could be detached and the muscle moved to behind the knee, as if it were a knee flexor. The tugs felt at the top end from hip movement may still cause the rectus femoris to react.
But now when it does, with its far end on the backside of the knee, it will not extend the knee but rather flex the knee.
Thus we can tap abnormal reactions and use them. When dealing with dense highly
stereotyped movement, cases in which sensory functions are typically also damaged, that is a good choice. The word "phasic" comes up in this context. It means that the muscle is being
driven solely by gross patterned mechanisms lacking the on-the-fly adjustment we normally enjoy. The patient probably is not capable of having his motor system duck below the
threshold of severe patterned muscle recruitment in cases where dense patterned movement is observed. That may well be the only type of movement (spasticity in series). But when the patient has less dense, less globally recruited movement and has sensory capability intact,
there are other choices.
The tibialis posterior (a muscle named for its dwelling place, behind the tibia - the shin bone) has a complex action of helping point the foot downward and - if unopposed - inverting the heel and supinating the forefoot. It can produce a club foot posture. In a spastic situation it may be totally active nonstop making walking most difficult. But move it to a new attachment, with a single short upward-only excursion - even without any helpers - and it can be reborn, not just active in the new job but controlled. It isn't the muscle that is "bad", but the neurologic circumstances under which it acts relative to the demands, velocity, number of actions, and number of stimuli etc. Change the rules, change the outcome.
General Strategies:
Arms:
Most upper extremity reconstruction for neurologic disorder involves muscle and tendon
transfer. There are few spare parts in the arm. If a well controlled arc of motion exists but points the wrong way, surgeons can rotate the segment to make it useful. We can combine
functions such as thumb and finger clenching into combined action to allow motors to be spared to provide missing release. One can fill a shelf of books with the many options. Just
know this: Without tactile discrimination (good sensation), it won't get used. If you want to know if muscle transfers SHOULD be done in a setting of poor function, if the sensation tests out as intact - do it! Just do it! Period!
With lesser levels of sensory discrimination (say "fair" on a standardized O.T. test), then you
weigh realistic surgical goals versus the demands of the process.
(You can click on the following images to bring up MPEG1 video.
If you do not have MPEG playing capacity in your broiwser, time to upgrade!)
Legs:
With legs, it is less critical that sensation be good to excellent. Even fair sensibility can be
made to do the less precise actions (compared to hands) involved in stepping. Even a rigid stable leg will be a benefit if the other leg can work with it, using it as a peg. As long as it
provides a reliable action that allows expectation of movement and outcome, it will get used. Thus the individual with dense rigid hemiplegia can still ambulate, if you just get the stiff leg
secure in stance in a balanced posture.
We can move motors up or down levels by working them backward. Examples:
|
|
Muscle transfers and recessions can reduce spasticity nearly as much as selective dorsal rhizotomy (SDR) in certain cases. Why this is so is discussed in the section dealing with mechanisms of spasticity, SDR, Baclofen, and alcohol blocks.
|
|
Because his sensory mechanism was so well spared he quickly gained standing and walker supported walking skills which advanced to crutch assisted walking. Interestingly, and unexpectedly (we're not THAT smart) as his muscle mass increased (from function), the alternate pathways of metabolism inherent in muscle began to reduce his acidosis to the point where he only occasionally required his "brew".
There are so many details and requirements for muscle transfers. We can not cover them all here. The main thing is to know that they exist and that what looks bad may very well be, but occasionally there are loopholes in disease.
Muscle transfers are used more commonly in the upper extremity.



