Selective Percutaneous Myofascial Lengthening,
(SPML)
Percutaneous Muscle / Tendon Lengthening
"SPLs"
"Percs"
"Gucci Procedure"
(and other nastier names)
 It would make sense to approach this subject historically. However, there has been much misinformation out there.
So let's begin with justification, our first consecutive case review reported some years ago at several national and international meetings with slight revisions as per protocols of the meetings (see, C.V.s) Reprinted
immediately below. Following is a plain-language overview.
It would make sense to approach this subject historically. However, there has been much misinformation out there.
So let's begin with justification, our first consecutive case review reported some years ago at several national and international meetings with slight revisions as per protocols of the meetings (see, C.V.s) Reprinted
immediately below. Following is a plain-language overview.
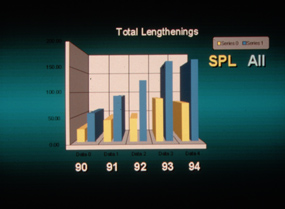
We have continued to tally and evaluate at intervals. Recent data is similar. This is the summation:
PERCUTANEOUS MYOFASCIAL LENGTHENINGS:
FIVE YEAR OUTCOME REVIEW
A different kind of muscle lengthening, initiated almost 30 years ago as a make-do in children with severe cardiac conditions, showed superior results leading to generalization of application. Gait analysis with telemetry emg evaluated those cases.
Length was initially derived from fields of disconnected small cuts (similar to mesh skin grafting) in the myofascia over the muscle surface. From the early observations, strategies evolved including : targeting high velocity muscles (attachment furthest from joint center as more stimulating of spasticity); avoidance of same session single joint muscles in ambulators (to preserve adaptive control mechanisms); avoidance of ranges of motion exceeding control capability (speed of response); and lengthening only palpably taut portions of the selected myofascia (commonly less than 1/10th of the width).
Our interest was most acute in the growing population. A five year consecutive review logged in over 500 patients age 12 years old or less at the time of surgery having this procedure in one or more muscles. They were divided into two groups. Those only having percutaneous myofascia lengthening and those having other procedures at the same session. In the group having other surgery, the outcomes totally reflect the diverse other procedures and are not the focus of this review.
The remaining group consisted of 278 patients with predominantly neuromuscular disorders who had only percutaneous myofascia lengthening (PML). The mean age was 6.5 y/o. Surgical sites ranged from 1 to 18 (modes 4 & 6). Parent questionnaire results were also included in the outcomes evaluation.
Results:
Post op admissions were 0.01% (4 cases, single night). Repeat procedures at any location were 10%. Recurrence of operative site contracture occurred in 7%.
There were no cases of infection, over lengthening, significant hematoma, nerve injury, nor dysaesthesia. All surgeries were performed supine. None required
surgical room time in excess of 60 minutes. Parent satisfaction was positive in 100% with similar follow up survey results one year later.
For those of you who are unfamiliar with topic of percutaneous lengthening, it relates to a type of surgery applicable to cerebral palsy, chronic illness, spina bifida, congenital defects, and various other reconstructive problems. It is an approach to muscle reactivity, range, and control. It is always designed with respect to the neurological control mechanisms, and although it is involved with creating length, length is not its singular goal in most cases.
'Percutaneous Lengthening' surgery was named well over twenty years ago; however, more recently the standard surgery done through smaller incisions has taken on the same name, creating confusion. Our original name choice for our procedure had been based on the skin rather than on the procedure itself - it wasn't well thought out, just happened. A physiologist at Johns Hopkins proposed the correct name: Selective Percutaneous Myofascial Lengthening (SPML). As we have trouble saying this, we find ourselves still calling it 'percutaneous lengthening ... be aware of this potential for confusion.
You may want to review neural mechanisms first. Let's review how this got started. Our percutaneous (tiny hole) method had nothing to do with cosmetics, although that was a
happy accident. We had a series of children with serious cardiac anomaly-related cerebral palsy. They either did not yet have definitive cardiac reconstruction or were being staged in one way or another.
When they walked, they turned blue. Walking is a high energy affair for many kids with cerebral palsy. Labored walking was in conflict with their cardiac status. However,
those same children were very serious risks for the routine orthopedic surgical interventions with the anesthesia requirements. Catch 22.
A way to partially or temporarily reduce the walking difficulty using local anesthesia and
not requiring intubation nor risky anesthesia positions was devised. It was based on the very same methods used by plastic surgeons to stretch small skin grafts over huge
burn areas but, in this application, was instead applied to deeper structures. The author had performed that skin surgery many times. It wasn't a stretch, imagination-wise.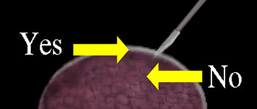
The children so treated ran circles around patients treated the other, standard, way. Gait analysis with telemetry (radio transmitted) EMG (detection of muscle activity akin to a cardiogram) showed very curious things. The most curious was that many large muscle groups that had been very overactive and badly timed were, afterward, well behaved - even though they had no surgery. The intervention had been directed at only the most over-reactive subset of muscles, in order to decrease the scope of the surgery.
At first, it was surmised that the walking disability of the cardiac kids was different in that it was amplified by their cardiac limitations (C3, compounding concurrent causes). So it seemed as if a little bit of surgery was all that was needed to get them below their cardiac limitation, and that's why they did so well so fast. But then, certain CP kids having noncardiac medical ills were also treated this way - again, to buy time. They, too, showed similar improvements in muscles not operated on.
It was clear that some central neurologic process was at work. It was not just superimposed cardiac limitation. Physiology basic science that we all had read, but didn't necessarily apply to tasks performed in rote manner, suddenly sprang to mind.
Reasoning on that, subsequent cases were given even more limited and targeted surgical treatment. The results did not suffer. Later cases revealed the additional problems of "control arcs" (see walking). The deep tissue techniques of percutaneous surgery were also applied to cases that were incidently having other open surgery so that direct vision got a chance to see what there was to see.
What was there to see? Nothing. Seeing does not help. There was much to be felt. Looking at a guitar, you can not tell if it is tuned until you pluck the strings. There are palpable strands in affected muscle that are not visible. Very tiny and very shallow centrally directed nicks cause them to give way and allow the muscle a much greater excursion without disrupting the continuity of the muscle. As surgical scope got smaller, the tools evolved also. Even the small laser probe became too big for the diminished need. Current tools are similar those used for eye surgery.
Selective percutaneous myofascia lengthening now seldom divides even 10% of the fascia in the limited subset of muscles selected in virgin cases. However, surgery is more extensive when scar from old standard open procedures complicates recurrent contracture. Scar from those old lengthenings is far more resistant to lengthening than the muscle contracture itself. We think that is why standard lengthenings have a much higher recurrence rate. It is the scar itself.
Another phenomenon caught our notice. There were children who had a certain degree of spasticity and difficulty walking and who were treated with standard lengthenings and who did well initially. With time, recurrence did not just lose that advantage. Certain of the children seemed to become worse than they were before their old surgery, even at less or similar degrees of contracture - worse neurologically. They seemed more spastic, more reactive, more sensitive to velocity. But that goes against the static neurologic damage theory of CP.
Our muscle transfer surgery uncovered the cause. In standard lengthenings, several muscles were approached through a single surgical plane. The fat between the muscle and tendon planes became replaced with scar which interconnected the deep plane (big) muscles and the superficial (thin smaller) muscles.
The superficial muscles travel further, by far, to their attachments and therefore travel further than the big deep muscles in any given functional movement. Spasticity is a response to velocity (via the spindle receptors in muscle). If slow moving large muscles get glued to the longer tendons of the superficial muscles, then big muscles get to move fast too. That means that a large VOLUME of spindle receptors cross the speed threshold that triggers spastic events. More fast moving spindles means more spastic. Spasticity is a second event. That's what the physiology basic science said all along. We just were not paying attention. First step - acceleration. Second step - reflex reaction to acceleration feedback.
First step, velocity crosses a stimulus threshold. Then second step, the velocity receptors bombard the spinal relay (internuncial cells) which recruit additional muscles which then also contract. The group spastic (second step) action of five muscles may well be triggered by a single muscle crossing threshold (first step). Think of it as fireworks. Stimulus goes up and an umbrella of activity comes down.
In performing transfers, it was found that the old surgical healing in the cases mentioned had not only cross connection but disorded tendon remodeling such that the long tendons had become common (the only) tendons as judged by the palpable lines of tension with motion.
It has become a muscle transfer strategy to get certain key muscles to velocities below recruitment level, that is rates that do not reflexly activate other muscles at a distance.
 |
Minimal scar has functional advantages. It is also much easier to revisit, if need be, at a
later time. It will not cross link fast and slow muscles.


Muscle tension and range are evaluated as the surgical process is underway. The operated muscle is not at rest, not still. Final tension and range are not a surprise but
rather the criteria of when to stop.
We often hear that our methods are only for the easy cases. Actually, we consider these techniques most effective in making impossible cases possible.
Examples:
 |
 |
This 19 year old girl had Wilson's disease for just over 9 months. She was nonambulatory even if assisted. She required special seating for inability to fully sit. She could not stand.
 |
Newer medications for Wilson's disease stopped progression. Percutaneous surgeries restored sitting, unassisted walking and, currently, jumping.
 |
Another teenager with Wilson's disease had extreme bilateral deformities of arms, hands, legs, and feet. Newer medications arrested the progression. Percutaneous muscle tendon procedures along with nerve block assisted casts returned him to walking independently and playing drums.
MPEG1 example [1.08megabyte file] (requires that your browser can enable MPEG viewing):
|
|
The first sequence, seen in the upper left inset, shows the initial exam with poor ability to stand erect against severe flexion forces. The lower right inset shows him very shortly after surgery. The last sequence, seen only in the video clip, shows him one year later with more skills under his belt.
Percutaneous surgeries have been used in a wide variety of disorders, from hemophilia, to brain injury, to complications of chemotherapy, birth defects, post trauma contractures, high tension electrocution and so on. Long-standing contractures of joints may require additional interventions.