Warning - deep stuff - for med students etc.
Background Information
Before the anesthesiologists get their part going let's give some background. There are four discussion areas in this topic.
1) What is anesthesia, in general? How does it work?
2) What differentiates pediatric
anesthesia from the main practice of anesthesia?
3) Tools of the trade.
4) Getting ready for surgery and anesthesia.
Analgesia: In general, analgesia is that which makes discomfort less onerous without blocking either awareness nor general sensation. Likened to listening to the radio pain station, analgesia works the volume control. In essence, those agents which dampen pain responses or our negative reactions to discomfort without shutting down neurologic pathways are analgesics.
Anesthesia: Anesthesia is that which cuts off sensibility. Anesthesia pulls the plug on the radio. Anesthesia shuts down neurologic mechanisms which convey sensory information. If that shutdown is of a region of the body then the anesthesia is called local. If it shuts mind down, then it is general. We'll see, below, that spinal is really a big local.
ANALGESIA:
No matter how obviously mechanical the pain cause seems to be - say a big gorilla with spiked shoes jumping up and down on your leg - that which we perceive is, nevertheless, chemistry. There in the leg, receptors get flooded with an extreme of mechanical change and signal s go out which are to be relayed as both localizing information and as level of damage.
But damage, itself, releases damaged tissue products which ought not be floating around free. That, too, sets a cascade of chemistry going. Some of that chemistry is set up to better allow blood vessels to deliver repair stuff. To that end, chemistry makes vessels leaky so that clotting goodies can plug holes. And some of the response chemistry is there to just punish you. It is saying, "Don't move me! Don't use me! And don't do that again!" Pain, in part, is nature's cast. But it is also an unsympathetic teacher with a switch in hand.
What is the chemistry of pain? It is very complicated, but we will give a skimmed down model. Just remember that the real story is much more detailed and varied almost cell by cell.
We discussed fatty acids in the basic science section. In short, a molecule which resembles the letter E, can attach three long molecular chains whose structures are built up in pairs of two carbons ("even chains") which end in a linkage*
OH
|
of O=C-carbon chain here.
That ending in water at body pH is polarized and called an acid. Carbon atoms have 4 attachment points. Those not used in making the carbon chain are capped with hydrogen atoms.
FAT:
E part fatty acids
___OH ... *\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\ The chains need not be equal length.
|___OH ... *\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\
|___OH ... *\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\/\
 Sometimes a carbon pair is double bonded (here not showing the capping hydrogen) as ...-C-C-C=C-C-C-... which is called unsaturated (saturated fats have more hydrogen). The unsaturated (double
carbon) bonds bend the chains and change the packing properties of these molecules in cell membranes.
Sometimes a carbon pair is double bonded (here not showing the capping hydrogen) as ...-C-C-C=C-C-C-... which is called unsaturated (saturated fats have more hydrogen). The unsaturated (double
carbon) bonds bend the chains and change the packing properties of these molecules in cell membranes.
The E part may have a phosphate hunk also attached which makes the assembly a "phospholipid".
One very important fatty acid is arachadonic acid. It is a chain of twenty carbons with four unsaturated linkages which fold the chain into a hairpin. This fatty acid is stored in (is a part of) cell membranes. It is everywhere. This fatty acid is freed by a liberator enzyme which unsnaps the fatty acids from phospholipids - a lipase ( say ly - pace).
Phospholipase A2 frees the 20 carbon chain called arachadonic acid (C19-COOH) which can be used by two interesting pathways of interest here. Aside from fat being burned (oxidized) as fuel down to free oxidized carbon as CO2, other oxidations can create weird molecules.
Two types of weird oxidation enzymes are:
Lipo-oxygenase and
Cyclo-oxygenase.
Lipo-oxygenase weirdness eventually results in arachadonic acid being oxidatively chopped and twisted into leukotrienes (say loo-koh-try-eenz. ...OK, don't say it, like I care).
Cyclo-oxygenase weirdness eventually results in arachadonic acid being oxidatively chopped and twisted into prostaglandins (pros-tuh-glan-din) and thromboxanes (throm-box-ayn).
The names are just names which give a clue to where they were first found and/or what they were first found to do [prosta from prostate gland, thrombo = clotting chemistry, leuko = white = white cells = inflammatory as army of white cells = pus]. Actions are many, as it turns out. Vasodilitation and constriction agents, bronchodilitation and constriction, gastric acid abating, and platelet joining agents are in these end products.
Aspirin goobers cyclo-oxygenase. Therefore, thromboxanes (clotting) and prostaglandins (lots of stuff including some pain amplifiers which increase sensitivity of the peripheral receptors) don't get made so well with aspirin floating around. The Non Steroidal Anti-Inflammatory Drugs (NSAIDs) work here. There are several steps in the very branched cyclo-oxygenase pathways mediated by helper enzymes. Thus, there is plenty to keep the pharmacologists up all night in the labs finding tweakers of this chemistry. But, at best, the chemistry related to pain in this pathway, amplifies but does not PRODUCE the pain response. Therefore super duper NSAIDS will not ELIMINATE the cry of pain, but just subdue the echo.
The interference with clotting of the aspirin-like drugs is the strong point (diminish over clotting as in heart attacks) and also the weak point (bleed and bleed and bleed).
Those agents that goober lipo-oxygenase block formation of leukotrienes which help call out the white cells. Thus they diminish inflammation. Some are used for asthma and the snots (rhinitis).
Acetamenophen is a kinda sorta NSAID but with differences. Despite claims, it is not as effective as aspirin in many key actions - but good enough where it comes to bringing down the amplification of pain (which is at the pain receptor location). Although it works in the cyclo -oxygenase milieu, its effects do not produce changes which goober clotting nor uninhibit stomach acid production. It is toxic to the liver in high dosage exposure. In diseases with substantial liver impairment, this must be considered. Also overdose is much harder to undo than with other NSAIDs.
"Oral" meds: "Puleeeeeeze! It tastes reeeel gooood, honey, baby, sweetie-pie. Mommy will give you all of your sister's possessions if you take this." Many of the oral meds are in fact able to cross mucous membranes in general. This is very convenient when kiddies refuse to open the top end or who ought not be taking anything orally. These agents are easily absorbed given in rectal form. Rectal acetamenophen is a commonly administered drug in the operating room.
LOCAL ANESTHETICS
Not amplifying pain is one thing. Blocking it requires shutting down the informational conduits to the brain - nerves.
Local anesthetics are chemicals which are placed right on a nerve and which make nerve conduction difficult to impossible. Maybe that's all we need to say.
No?
OK. The first local anesthetic was a beast. It was fiercely vasoconstrictive and produced euphoria to the point that the pesky numbness it also left behind was tolerated. That vasoconstriction - of cocaine - is so intense that snorters shut down blood flow to the nasal passages to the point that the tissues in there die - dead - bonkers- kaput - and slough away. That's why they have those sunken in mid faces and quicksand noses. The famous surgeon who first really promoted this stuff for surgery also got really hung on it.
But chemists are chemists. The nerve deadening unfun part could be exploited and the euphoric vasoconstrictive aspects eliminated by tweaking the chemistry.
 At the heart of it we again go to cell membrane chemistry. In this case, we recall that a cell membrane
is a mini peanut butter sandwhich. The surfaces are water friendly (hydrophilic, say Hy-drow-fil-lik) and the center is hydrophobic.
At the heart of it we again go to cell membrane chemistry. In this case, we recall that a cell membrane
is a mini peanut butter sandwhich. The surfaces are water friendly (hydrophilic, say Hy-drow-fil-lik) and the center is hydrophobic.
See cell membranes for more on this.

The local anesthetics have short structures with three regions: Oily-link-watery (in tech talk: hydrophobic, intermediate, hydrophilic). The "caine" ending of most of their names harkens back to the first member of the group - cocaine.
Cell membranes having a triple property surface in the form of a membrane with  water-oil-water layers prevent willy nilly passage of most
things in and out of the cell. Think of it as plastic wrap. But there are holes all along the membranes with specially configured doors that allow guarded passage in or out. These protein gates are fairly
complex structures that may be assembled from even eight proteins or with complex foldings of tails that anchor the "pores" in place in the membranes. Specific doorways - or gates - or most popular CHANNELS through the cell membranes which interest us in this section are the sodium (Na++), the potassium (K++), and the chloride (Cl=) versions.
water-oil-water layers prevent willy nilly passage of most
things in and out of the cell. Think of it as plastic wrap. But there are holes all along the membranes with specially configured doors that allow guarded passage in or out. These protein gates are fairly
complex structures that may be assembled from even eight proteins or with complex foldings of tails that anchor the "pores" in place in the membranes. Specific doorways - or gates - or most popular CHANNELS through the cell membranes which interest us in this section are the sodium (Na++), the potassium (K++), and the chloride (Cl=) versions.
Cells, especially nerve cells, keep a very high inner concentration of potassium and float in a sea of outside salt water ( Na++Cl= ). The difference in concentrations creates a battery, a charge which would quickly equalize if only those channels would open. When one channel does open the ions (sodium etc.) seek to equalize. In-out reversals of Na and K and Cl toward equality cause loss of charge. That tweaks the neighborhood molecules of the cell membrane and cause the nearest channels to also open. A wave of opening channels spreads away from the one that first opened.
Immediately, cell chemistry is set into play to "Scotty! We need shields! Now!" "Captain, ahhm doon thuhbest agh cannn!" and the wave of open channels is followed by closings. The cell madly pumps the sea flood right back out and uses energy to attract potassium. Sodium is once again outside and potassium inside and the charge is reset across the cell membrane once again.
That wave of depolarization (loss of charge) is a nerve impulse. That's how we think, I think. Who said, "I think, therefore I am depolarizing?" (They keep leaving off the last bit).
 Anyway, local anesthetics whose last name is 'caine' goober the
sodium channels. Those doors get stuck. Two ways. One is adjacent the doors in the membrane buggering the door opening elbow room.
Anyway, local anesthetics whose last name is 'caine' goober the
sodium channels. Those doors get stuck. Two ways. One is adjacent the doors in the membrane buggering the door opening elbow room.
The other is in the door opening itself - a cork.
Either way, or both => no flow.
No flow - no go.
No go - no know.
No know - no pain.
No pain and no gain (in the electrical sense meaning amplification).
Interestingly, as these drugs can affect happy cells as well as sad cells, keeping the action local means putting the local anesthetic agent right where it is needed. Needles. Recent developments have included topical goo versions which allow tearless use of needles. That really requires at least 45 minutes of application and better 90 minutes. Translation, getting there way earlier than the procedure that is scheduled.
Local anesthetics are metabolically degraded. But to keep larger injected doses from diffusing systemically with distant effects (like seizures) before they are degraded - local vasoconstriction is sometimes employed. Shades of cocaine? No. Epinephrine is used for that effect rather than pervert anesthetics back to the old nasty stuff. Epinephrine, added to decrease toxicity, also prolongs local action. It may also slow onset of numbness a bit by slowing the diffusion. Some nerves are wrapped in layers upon layers and layers of fat. These myelin covered nerves are very big with all that insulation. That covering allows a special kind of depolarization that hugs the nerve and travels much further much faster.
This writer broke his foot and heard the crack, recognized the source, and identified the location by its feel all before that nasty clobber of pain landed in the brain. The pain fibers - mercifully - are not the big fast well insulated ones. Sometimes local anesthesia allows you to feet bits of touching here and there yet with no pain. Reason - insulated fibers, which carry localizing information, have not been fully penetrated.
To penetrate all the nerves, the chemistry of those thick coatings had to be penetrated by the local anesthetics. That's why there are so many kinds, and why the pH of the anesthetics is so important to how they work.
Examples: topical benzocaine, very fast lidocaine, very long acting but slower onset bupivacaine. Surgeons may begin with a fast acting and finish up with a long acting local anesthetic placed with the help of a topical. Polarized molecules swim fast in water but don't penetrate fatty tissue. Uncharged molecules zip through fat & myelin but move slowly through water.
"I want 16 things done - all under local"
Local anesthetics in lots of places at one sitting? Here, toxicity limits us. We know just how much of any agent is safe. If you want to cover more ground than combined local dosages would allow (and for longer periods of time), then fish upstream. Spinal anesthesia is just local anesthesia injected higher up. As some liquids can settle or rise in other liquids, the local anesthetics used for spinal anesthesia have been made to either rise or settle or mix well when injected. Side lying spinal can therefore just numb one leg and spare the other - and more importantly - spare many of the reflexes needed for faster recovery (like urination).
Because some of the post operative responses are mediated by pesky spinal reflexes and because general anesthesia may turn the brain off but leave those unaltered, local is often used as well as general anesthesia for local reflex control in some complex surgeries. There are other methods as well, though.
Seeping Flow:
The coverings of nerves are discrete tissue planes that allow fluids to seep. Large volumes of injection near a nerve WILL travel along the surface of the nerve to wherever that nerve is traveling. For that reason small volume injection is favored when only a local action is wanted. In fact, military field anesthesia employs the reverse. A needle probing gets a nerve response in the leg to show the needle just touched the nerve. A pint of fluid with local anesthetic dispersed within it is then allowed to flow into that seemly isolated place. Within about ten minutes both legs go totally numb. This is a spinal anesthesia via the front of the leg. That flow along nerves also explains why long term nerve blocks had such bad press in the old days (before the electrical tools were available to precisely isolate nerves and allow efficacy with tiny injection volumes).
GENERAL ANESTHESIA:
So, just make the brain not conduct nerve impulses and you have ....
... a real mess. It's called a code.
This approach requires subtle selectivity. Very subtle. Slightly mess up some parts of the brain's conduction but not other parts hardly at all. Slugger on-off drugs just won't do. Big cork like molecules? No.
 What does work?
What does work?
Subtle molecules that nestle gently into fat (the lipid or fatty inner layer of the cell membrane) and nudge a bit. That property is common to central acting feels-good drugs (including barbiturates and booze) and general anesthesia.
Most general anesthesia chemistry is simple stuff that dissolves in oil. The anesthesia gasses (labeled as An in the image at left) are actually liquids (exception being nitrous oxide which is a gas at room temperature). Nitrous oxide comes in a gas tank as you would expect. The others come in glass bottles.
 However, they are delivered as gasses the same way grandma
delivers that savory smell of food from the kitchen.
However, they are delivered as gasses the same way grandma
delivers that savory smell of food from the kitchen.  They're cooked
and give off vapor. The vapor pots are a bit specialized to exactly deliver so much vapor. So we see one pot per anesthetic agent.
They're cooked
and give off vapor. The vapor pots are a bit specialized to exactly deliver so much vapor. So we see one pot per anesthetic agent.
The vertical glass tubes are flow meters which show mechanically what the mix of 'gas' and oxygen is. There are also electrical sensors but mechanical redundancy makes the delivery system able to keep going if electricity fails. The gas mix going in AND that coming out is monitored for content.
 Fat soluble liquids? Sound familiar? The early anesthesia gasses were pretty car and jet good fuels. They could make a car go, a plane fly, and blow the walls out of a
large building if mixed with oxygen. Anesthesiologists are particularly fond of oxygen. Let's see. Take this very explosive gas, like ether, mix it with a high concentration
of oxygen, surround this mix with all manner of electrical devices and sheets rubbing on blankets and you have --- all those pesky hospital building codes, funny dress, and
static electricity avoidance practices. Did you notice the odd flooring and chains hanging off nearly everything?
Fat soluble liquids? Sound familiar? The early anesthesia gasses were pretty car and jet good fuels. They could make a car go, a plane fly, and blow the walls out of a
large building if mixed with oxygen. Anesthesiologists are particularly fond of oxygen. Let's see. Take this very explosive gas, like ether, mix it with a high concentration
of oxygen, surround this mix with all manner of electrical devices and sheets rubbing on blankets and you have --- all those pesky hospital building codes, funny dress, and
static electricity avoidance practices. Did you notice the odd flooring and chains hanging off nearly everything?
Real people really did blow up sometimes. But what else was there? Chemists to the rescue. Nonexplosive versions. Oxygen is a very very reactive and nasty substance chemically that just rips in to many things. Thus we get rust, flaky gray aluminum, lime, and forest fires. But chloride is right there too, as a nasty oxidant, that is. Thus bleach. The nonexplosive anesthesia agents use chlorine or kindred fluorine or bromine oxidants instead of oxygen on the molecules so that pesky oxygen won't try to take over the anesthetic molecules in explosive oxidation. That's why the anesthesia agents are "halogenated". Halogen is the chemical grouping of similarly reactive chlorine, fluorine, and bromine - powerful oxidants in their own right.
The chemists also figured how to deliver anesthesia inducing cell membrane oil layer nestling molecules from within a water delivery medium. So general anesthetics can be delivered as intravenous injection as well as breathed vapor. The injection forms require water dispersing hand-holding chemistry to keep the oils from separating. That is what soap does, by the way. So it is no surprise that these intravenous anesthetic agents look soapy or milky.
There are, too, those chemistries that don't so much disturb nerve transmission along the nerve but rather transmission from one nerve to another. Neurotransmitters are simple chemicals that are released by one nerve after the depolarization wave hits and which, on release, open specialized channels on the next nerve. Transmitters can amplify and sustain transmission of messages or they can be inhibitory. Indeed, much of the higher acts of consciousness get their precision from inhibitory circuits. Things are not just what they are they are also not what they are not. Conscious distinction goes beyond definition. Refinement is found in exclusionary processes. Looks like a horse, gallops like a horse, but horses aren't striped... not a horse...
Known neurotransmitters include acetylcholine, norepinephrine, dopamine, serotonin, gama amino butyric acid (GABA), glycine, glutamic acid, aspartic acid, and a few others such as encephalins and substance P. These are the batons passed between neurons - one to another.
Dopamine, norepinephrine, and serotonin are collectively called monoamines (one amine in the molecule). Norepinephrine is a reticular (deep spooky part of the brain) transmitter which is widespread and inhibitory. Yet, norepinephrine given in a flood is stimulatory behavior-wise. The reason is that it is inhibitory - chemically - of pathways that are inhibitory functionally. Inhibitory of inhibitory. See? It is pretty messed up when spoken about in generalities. Anesthesia agents are not given here or there but as generalized floods. The same agent may be stimulatory of behavior and then become inhibitory as different circuits with different sensitivities kick out in sequence.
From this we get
The Stages of Anesthesia:
Stage I - general analgesia - very zoned, goofy to stoned
but some feeling intact and other sensation missing
Stage II - excitement - actually unconscious and amnestic (won't
remember anything here), but appears more alert with vigilant thrashing.
Will pull at face and objects. All reflex.
Stage III - surgical Anesthesia - asleep and comfortable but al the good stuff
is working. There are sublevels with less and less reflex and respiratory
autonomy
Stage IV - Vital Paralysis
Important stuff is no longer controlled. Vascular tone is on its own and not likely to correctly control flow distribution to the various parts of the body. Blood pressure can just drop away as control over the tone of blood vessels goes limp. Stage IV is also called too deep. Electrical stimuli that cause twitching (reflex) are often given and monitored to be sure that this stage is not entered. There are many subtle signs that tell the anesthesiologist of the depth of anesthesia. They vary with age and body size to a degree, especially with regard to sensitivity.
Relaxation:
So, when muscles need to be loose to perform certain surgical maneuvers, the depth of anesthesia can be deepened - or - muscle activity can be turned off directly from a safer level (or stage) of anesthesia using muscle turning off drugs.
Just as there are neurotransmitters there are similar goodies that transmit from nerve to muscle . Some drugs block the neurotransmitter from getting at its receptor on the muscle. Thus the muscle will not "fire" (that is, depolarize) as the neuromuscular transmitter can't get into the receptor. These are called nondepolarizing blockers. Natives shooting monkeys out of trees with darts found this group of agents (curare and such).
Another group of agents depolarize the muscle at the special receptor then don't let go - but just hand in there. The depolarization is then way prolonged then the muscle peters out in the depolarized state, unable to recharge for the next go round. These are called depolarizing blockers. Succinylcholine is an example of that. The first thing seen is a tremulous activity of muscle and even fine writhing tension followed by limpness.
There are certain rare persons whose family has a chemical oddity that makes these drugs very undesirable. The action of these drugs may make the muscle go bonkers and nearly self destruct in huge metabolic outpouring which can flood the body with released potassium and oxidize fuel so rapidly as to induce immense fever. Malignant hyperthermia is a risk suggested by a very exaggerated tendency to fever from other causes. "You know, we almost lost grandpa to a single whiff of anesthesia." Profound and sustained motion sickness is sometimes a clue. Some sheep with the identical condition will die of transport by train. I don't think it requires that they ride backwards or read the newspapers, either.
Tools of the Trade:

You.
 We already saw the anesthesiologist's stove with its cooking pots.
The gas mixture is delivered by a crinkly hose with a squeeze bag (here green) attached.
We already saw the anesthesiologist's stove with its cooking pots.
The gas mixture is delivered by a crinkly hose with a squeeze bag (here green) attached.
It is the job of children to try to blow this balloon up so far to pop it right off. The girls think they can do this better, but the boys are not so sure...
While that contest is ongoing the canister behind it is removing expired CO2 from the out breathed gasses . The material turns color in
the process and gives another measure of the metabolism process.
. The material turns color in
the process and gives another measure of the metabolism process.
The face mask is like the ones used by pilots. It is soft and fits over the nose and mouth. Sometimes it smells like bubble gum or strawberries or any tasty odor that you may want your child to come to hate.
 The hose delivers the perfumed sweet air (laughing gas - now don't giggle too
much). It also carries away the breathed out left overs. There are valves and make it go one way and thingies to keep the air warm and moist.
The hose delivers the perfumed sweet air (laughing gas - now don't giggle too
much). It also carries away the breathed out left overs. There are valves and make it go one way and thingies to keep the air warm and moist.
Phoof huh phoof huh phoof ...
...almost got that balloon blown off... any second now...
Getting harder, mellow, whoa who cares... girls ain't so bahhhd..
Stage II - ripping at mask and legs struggling!!! What's wrong? Why's he struggling? That's stage II which is nice to get through quickly. It is the stage that makes many docs wish parents were not there - as they might not understand how normal it is and not a discomfiture. That struggle is all reflex and done from an unconscious state. If you can't deal with that - then don't put yourself through parent in operating room trauma.
Stage three - resting quietly with even a smile - maybe. Hey, he's awake. His eyes are open. No. It's just that the lids can't close of their own. We do that with a bit of tape. But first some goo to keep them moist. Nurses will wash out all the goo that anesthesiologists put here and there to keep stuff from
getting dry. Give her a big kiss, Sumaaaackpfffffuffft. Good one. Now go to the waiting room and worry. That's your job. But distracting flow in the OR is not in the child's interests. Go.
No. It's just that the lids can't close of their own. We do that with a bit of tape. But first some goo to keep them moist. Nurses will wash out all the goo that anesthesiologists put here and there to keep stuff from
getting dry. Give her a big kiss, Sumaaaackpfffffuffft. Good one. Now go to the waiting room and worry. That's your job. But distracting flow in the OR is not in the child's interests. Go.
This next part is pretty gross. That mask on the outside of the face is
OK. But it can drive anesthetic gasses into the swallowing pipe (esophagus) if the airway isn't supple, or if the throat valves are not  optimum, or if a whole bunch of stuff. This smaller sits INSIDE the mouth at the back of the throat. It
holds the tongue out of the way and inflated pretty much blocks off the swallowing pipe - delivering better to the lungs and less to the stomach. Laryngeal Mask Anesthesia is referred to as LMA.
optimum, or if a whole bunch of stuff. This smaller sits INSIDE the mouth at the back of the throat. It
holds the tongue out of the way and inflated pretty much blocks off the swallowing pipe - delivering better to the lungs and less to the stomach. Laryngeal Mask Anesthesia is referred to as LMA.
The older kids may notice that their throats feel scratchy
later on. That goes away. But what if the child is going to be turned face down? Or, what if the operation is going to be very long, or if the chest is a target of the surgery? Or a whole series of other stuff?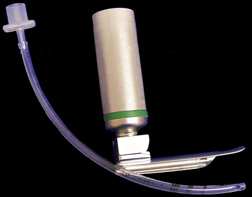
The endotracheal tube is a plastic tube that fits directly into the windpipe. Bigger kids may have a tube with a soft balloon over the end section for better seal. It has to be soft to not cause pressure on the delicate tissues. The tiny kids get very exactly measured balloon free tubes as seen here. The right sized tube is just about the girth of the small finger. That silver thing is a fancy flash light with a tongue blade so that the anesthesiologist can place the tube in the wind pipe under direct vision.
Endotracheal tubes (endo = into the) are apt to be used when trauma requires anesthesia with no chance to empty the stomach. The anesthesiologist will also, later during the surgery, when things are less hurried, pump out the stomach. In that case a tube is snaked into the stomach and suction is used to remove contents. That tube may be removed or left in place depending on what is going on.
 One thing that ought to be going on is oxygen getting from the lungs
into the blood. That is supposed to happen, but it is nice to be sure and know how much. Facial color is fine. But a nifty red light with a sensor to see how much gets color shifted can tell exactly how
much hemoglobin is carrying oxygen. Oximeters can
One thing that ought to be going on is oxygen getting from the lungs
into the blood. That is supposed to happen, but it is nice to be sure and know how much. Facial color is fine. But a nifty red light with a sensor to see how much gets color shifted can tell exactly how
much hemoglobin is carrying oxygen. Oximeters can ![]() be used on
fingers, toes or the ear.
be used on
fingers, toes or the ear.
Chest sticky pads are placed to pick up heart signals and measure the heart rhythm. Mechanized blood pressure cuffs give a running trail of blood pressure readings.
Red Heads, eye balls, and chubby children:
or
"When the *ell is he going to wake up?"
Eye surgery is notorious for making nausea. Specific anesthesia agents get blamed when the real culprit is what wasn't given. Certain agents can head off this reaction to a large extent.
Red heads are cute. We all agree on that. Right? And they puke their little red heads off way more than brunettes. Blondes are in the middle. Nobody knows why. But if this writer had to guess, it would be related to the fact that melanin (the stuff that makes us tan or black) is made of the same stuff that is used to make most of the neurotransmitters. Maybe not.
Now, remember that nearly everything that makes you snooze dissolves in fat? That means that long procedures will saturate body fat with anesthesia agents. Body fat is a reservoir for these agents. The more body fat the longer it takes to wake up as anesthesia agents seep out of body fat stores rather slowly.
 |