|
 Chronic Shock Chronic Shock
Syndrome
& the
Art of Medicine
This is not a new subject by any means. It is actually quite old. It is simply somehow not well represented in "the literature". It is what the old
timer surgeon tells the younger residents who are about to make some terrific mistakes based on what the lab is seemingly telling them about a patient.
This is the ART of medicine which so gets little due in an age that worships decimal places even if totally misguided. It is scientific to be wrong as long as you are wrong to seven decimal places.
The Art of Medicine - short & sweet:
I was a general surgery resident and my chief overheard me asking a sweet teenager if there was even the
remotest chance that she could be pregnant. She assured me with great emphasis that THAT was impossible. I continued through the litany of other medical presurgical questions.
My chief pulled me aside and asked me in a pressured disbelieving way if I really asked THAT particular question? (or just a list check off?)
I asked it. Yes. Why?
WHY???? He was wide eyed in disbelief.
I asserted, It's important! Why would I NOT ask her?
BECAUSE YOU MIGHT BELIEVE HER!!!!!!
And, yes, her life was saved by expertly handling an ectopic pregnancy.
See? The art of medicine considers reality and reality is complex and not always to be relied on for truths. And
even when people tell the 'truth' the fact is they are wrong as often as not.
But laboratory data can mislead as well. Chronic shock is a common special case for those of us who treat
people with chronic disabilities.
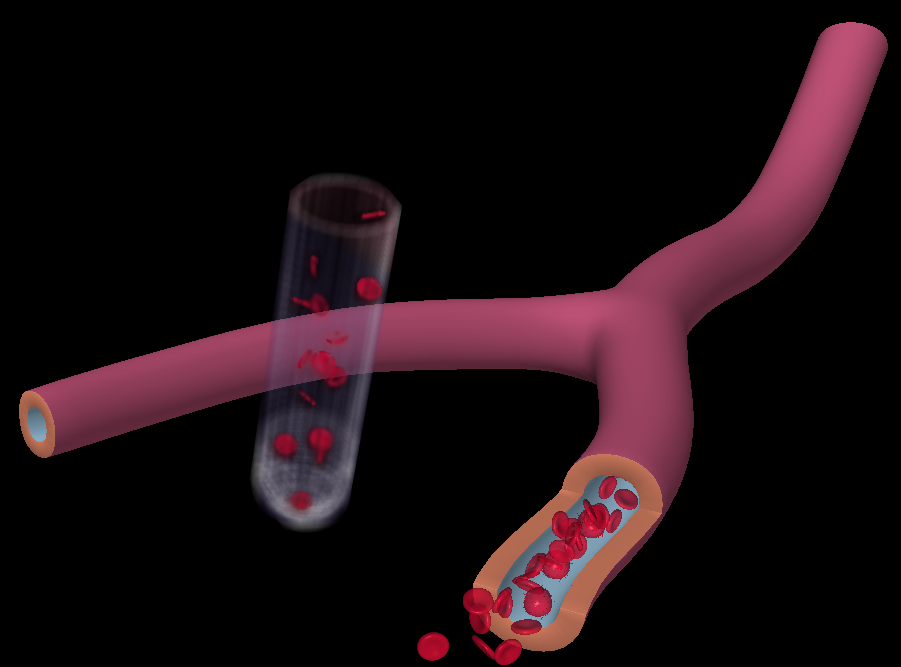
Simple anatomic fact. Normal veins are bigger than and outnumber arteries. The venous tree (veins) carry six times more blood volume than arteries. Arterial pressure does the work of supplying nutrient & oxygen need as
well as a variety of protective goodies, driving that stuff through tiny tubes. Veins just complete the circuit return to base at a much lower pressure and with slower return and much bigger volume by 6 times. This
venous volume excess is a safety against blood pressure drop or overt loss. It also assures that there is enough of
many required goodies circulating to get certain jobs done - such as clotting.
Lab tests measure a blood sample for its relative content. So much sodium, so much potassium, so much
prothrombin, fibrinogen, platelets, white and red cells and so on in a given volume sample. It does not measure what actual volume is.
So the tests do not tell you how much blood, in total, is actually circulating. Doctors calculate THAT volume from body weight as a quickie estimate or closer from height and weight calculations or a chart.
Could that calculation and could that chart be just plain wrong?
Yes.
If the hypothalamus is a bit off, or if the patient can't communicate well, slowly over a long period, a deficit of
water intake - simple drinking of water - gets offset by the venous mechanism of making-do for loss. As if
there were bleeding, the venous tree contracts. The arterial side maintains pressure. So measured items as
RBCs and sodium all are normal in value (concentration). But actual circulating volume may be dreadfully low.
When venous volume approaches arterial volume there is no more making-do and the patient can crash. That is very rare.
But if a lesser degree of venous volume drop is paired with a vasodilation as might occur with anesthesia - it can
behave as if there had been a sudden loss of units of blood volume. An operation that lost little blood might suddenly require a transfusion to maintain stable vital signs.
Hey! THIS IS COMMON IN HIP SURGERY!!!!!!!!!
But after-bleeding might also be seen. Normal concentration of fibrin in too little total blood is simply too little
fibrin for the job at hand. So the cut tissues ooze blood again, even after they seemed to have clotted properly.
It can be misinterpreted as coagulation process run wild depleting fibrin. Certain infections can do that. There are other things as well to keep people guessing.
When fluids are given and the venous tree gleefully (in a venous sort of way) accepts that long overdue volume
the absorbent content of the blood may be too low to maintain that returning fluid just arriving into the vessels.
The fluid may ooze out into and between the tissues (the "third space") almost as fast as it gets put into the veins.
Eyes then get puffy. Limbs look waxy and wound swelling seems a bit exaggerated. After three days the body generates more protein with fluid absorbency into the vascular system and that swamp of leaked tissue fluids
gets sucked back into the vascular tree. At that point the blood counts seem to be falling! RBCs are going
down - in concentration, but not in total. The risk is that a transfusion, responding to a falling RBC count, may overwhelm an already rising but unmeasured volume and lead to pulmonary edema.
The surgeon is avoiding all this because she was looking at urine output and quality. A dense yellow
color means that the kidneys are holding on to water - circulating volume is probably low. When the urine
output suddenly rises and third space water is now flowing back into the vascular tree, the urine starts looking
like tap water. Dropping sodium and potassium and blood count but high urine volume with tap water like urine is third space coming back into the circulation in order to to be rid of by the kidneys.
Too technical? OK. That's what makes surgeons - surgeons. But look. See the basic fact that screams out? BEFORE the surgery, well before the surgery, simple drinking of water can tremendously improve
healing, clotting, and avoid blood transfusion.
THAT is a fact that needs to be in the HOME. People in wheelchairs - as a group - simply don't drink enough
water. That can lead to death in more ways than can be listed in polite language. A preop urine test, in the face of everything else normal, showing concentrated urine can be a scream for help.
|
