 |

Lordosis may be accentuated in syndromes to the point of being unsightly. There may be combination issues. For example, the skeletal growth may include oddities that cause excess lordosis. However, weight alone may be the larger factor.
We all know the pride of pregnancy, yet another name f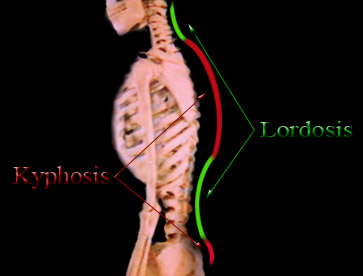 or lumbar lordosis with an upbeat spin. Beer belly has a negative
connotation. The posture is similar. Back ache is commonly experienced when lordosis is excessive in the low back because the vertebral bodies, built for support, are no longer bearing the load.
or lumbar lordosis with an upbeat spin. Beer belly has a negative
connotation. The posture is similar. Back ache is commonly experienced when lordosis is excessive in the low back because the vertebral bodies, built for support, are no longer bearing the load.
 Instead weight is shifted back onto the posterior elements whose job it is to steer, not support.
Instead weight is shifted back onto the posterior elements whose job it is to steer, not support.
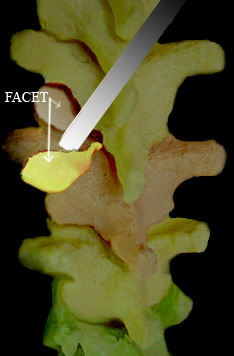
By dividing a portion of the poster element from the backside of a vertebra, we expose a facet joint.
These small joints (small joints = facets) which overlap like shingles on a roof, forming the back surface of the spine when compressed long and hard get gnarly and hurt. That hurt radiates very much the way disc rupture pain does. It is a more common source for sciatica pain than the sciatica caused by disc rupture (about 10:1 ratio).
OK, so there is good looking lordosis, exaggerated lordosis, annoying lordosis and even painful lordosis. But forces of nature rarely stop with the merely interesting.
Occasionally it can be so severe as to present itself as a mass protruding from the abdomen. It can be mistaken for an anneurysm as the aorta is carried with it and a pulsing bulge is noted pushing forward through the belly wall. That isn't a pure event, though. It is seen occasionally in paralytics whose balancing forces can go wildly awry.
Lordosis - Surgical Degree
When normalcy is lost to PROGRESSIVE curvature, not just a posture or a shape but rather a PROCESS , then it is rather like scoliosis. That is, it is progressive spinal curvature with which we must contend.
When the conservative measures fail, then the interventions seem rather akin to those of scoliosis. Here is an example.
 This girl with cerebral palsy had a selective dorsal rhizotomy performed about 8 years before. At that time, a long posterior opening into the spinal canal unroofed
about 6 vertebral levels. That segmented bone was put back. Unfortunately, those bones spontaneously fused into a single block.
This girl with cerebral palsy had a selective dorsal rhizotomy performed about 8 years before. At that time, a long posterior opening into the spinal canal unroofed
about 6 vertebral levels. That segmented bone was put back. Unfortunately, those bones spontaneously fused into a single block.
In other words, the six vertebral levels joined posteriorly and became a tether to posterior bone growth. Because the front of the spine continued to grow, a severe lordosis developed. Seen here it is a lordosis the end vertebrae of which are 115 degrees to each other. That number is so severe that even if growth stops, gravity will continue to increase the deformity.
She had significant difficulty with seating, but pain was the reason for seeking surgery.
CT scan showed what was feared, that spontaneous fusion had taken place. That fact was not apparent from x-rays alone. A single side anterior 'correction' could easily fail as the posterior fusion could be quite rigid.
 Surgery was Back-Front-Back.
Surgery was Back-Front-Back.
In one surgical day under a single anesthesia, the spine was exposed from the original neurosurgical route (posterior).
Multiple osteotomies (dividing of bone) reestablished the discrete levels of vertebral planes of movement. The posterior wound was closed.
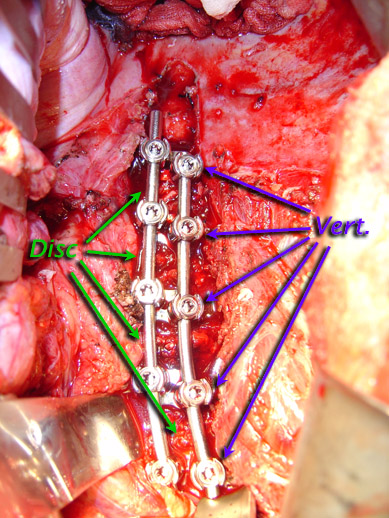
Then from the front, disc removal allowed correction of the deformity.
In this case, double vertebral screw fixation was selected to allow better fore-aft tilt control and strength. On the side of each vertebral body sits a staple tamped into place. That staple bears two holes. Through each hole is passed a vertebral screw.
Vertebral screws have advanced spinal surgery tremendously. They were the target of litigators looking for a new breast implant like cash cow. Fact is, pedicle screws have salvaged people we never thought were even to be given a prayer. Even when the bone anatomy in the back is poor, these allow significant holding power to secure the spine, reshape it and hold it until healed.
The rods are placed and adjusted sequentially until the desired curvature correction is attained.
Bone chips in the spaces where disk was removed assist fusion - although those spaces are closed flat. Additionally some anterior vertebral bone adjacent the spaces was removed to promote the desired closure angles.

An x-ray from back to front (a front view seen to the right) looks like this. You can see the pairs of screws going from patient left pointing toward right passing through the vertebral bodies.
Once the abdomen and chest cavities are put back to rights, with the diaphragm repaired, and the skin closed. The original posterior wound is reopened. 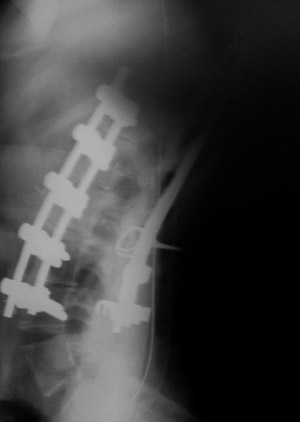
Blood scavenging devices which were left buried are removed.
The posterior spine is now instrumented.
From a side view x-ray (on the left) we see that the severe lordosis is gone, leaving a normal degree of lordotic curve in its place.
The patient is quickly mobilized to seating posture in the postoperative period. She appears to be and feels taller.
 There is lordosis, bad lordosis, really bad lordosis, and then there is this. With spina bifida, deformities ought to be addressed
early because no matter how bad it has gotten, it can still get worse.
There is lordosis, bad lordosis, really bad lordosis, and then there is this. With spina bifida, deformities ought to be addressed
early because no matter how bad it has gotten, it can still get worse.
Given really bad skin and poor soft tissue coverage, it makes sense to address this helical lordotic scoliotic curve in the main, from the front.


