|
|
||||||||||||||||||||||||
|
The term hemiplegia does more to confuse real understanding than nearly any other poor medical term. It just means one side of the body. By default the more typical adult stroke pattern is what comes to mind when that term is used (but those strokes vary). When you say hemiplegia you are, whether you mean it or not, implying a stiff side of the body with a stiffly extended leg, a withdrawn elbow and hand, with arm and hand involvement worse than leg and with substantial loss of sensation or involvement of that side in knowing and doing. Sometimes you see those features in kids with diplegia (PVL) and they get called triplegia. We would rather say that there is PVL with an additional stroke or diplegia plus hemiplegia because that gives a very sharp image of how the parts behave. MORE important - it gives us a good edge on how they will behave if we tamper with things. Oh, and yes, we can have half of a hemiplegia (lower or upper). Where did the brain get injured? How extensive? More than one spot? And are you aware that more babies have strokes than adults? Mmmm?? That's another subject. Injuries tend to be mechanical and focal (vessel plugs and its territory dies, or vessel bleeds and the blood pressure kills tissue). Group 1.
We will break the problem into groups according to not what is wrong, but rather what is working or has potential to work (sound familiar). Basically two main groups with details to mop up in each. . .
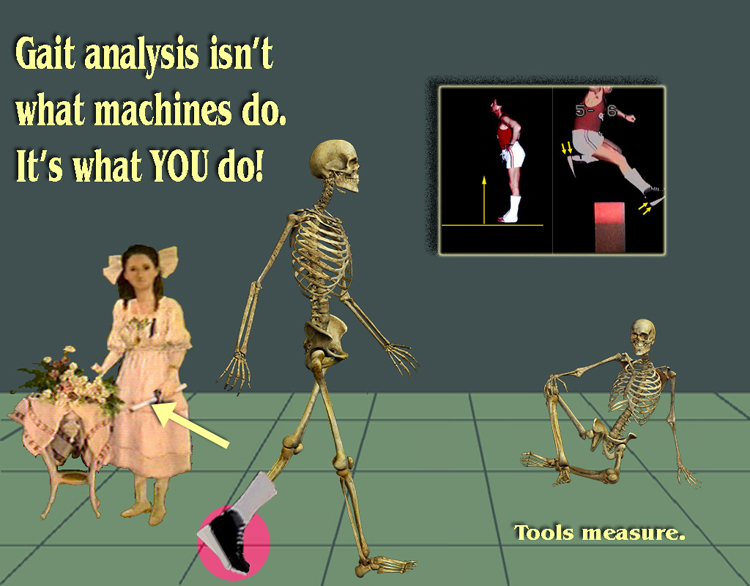
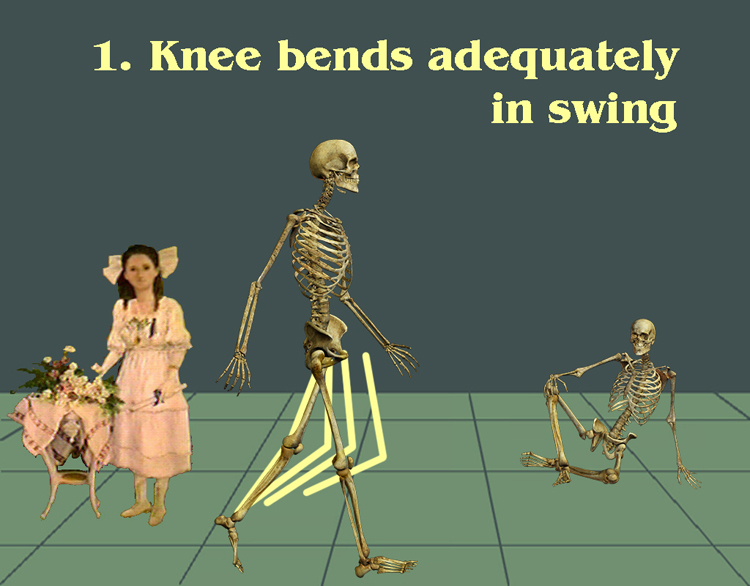
Got that? SWING! LOOK AT SWING! The stiff stance is a distraction. Does the stiff leg bend in swing phase?
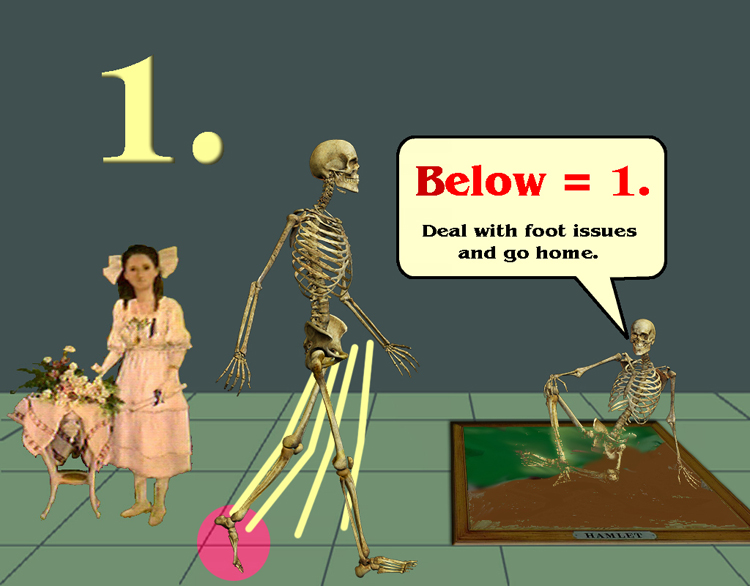
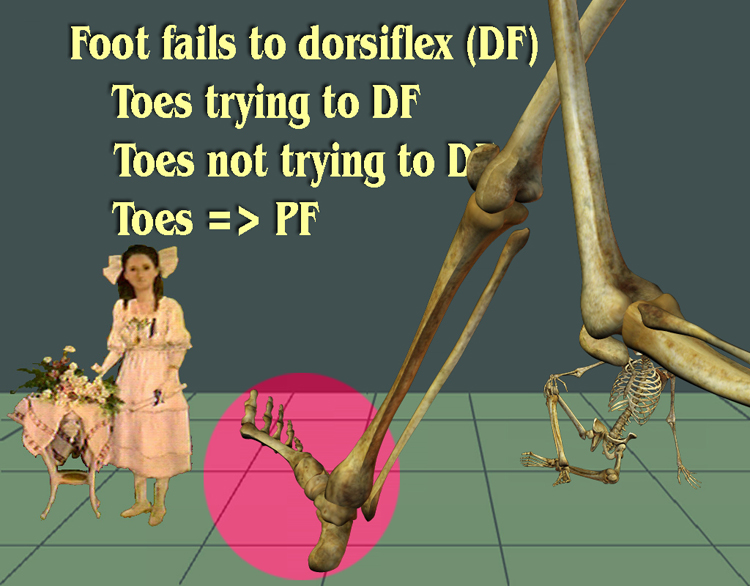
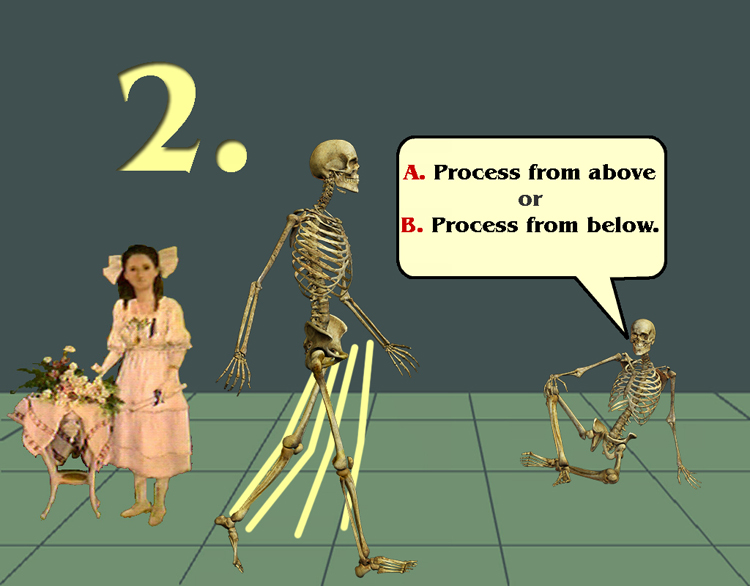
A hanging down foot means you have to bend the knee more than normal or swing it outward weirdly. And it means that stance will be stiff as the foot plants toe to heel and drives the knee backward (back thrust, or recurvatum, or back knee, whatever). Group 1-a = things are trying to lift the foot (toes pull strongly upward trying to get that foot up). Group 1-b = foot is down and nothing seems to be trying to do anything about it.
So group 1 is good. Fix the foot and function is near normal. (We can fix the foot). 1-a&b is lengthen calf musculature ('Achilles', gastrocnemius etc.). 1-a maybe done. If foot elevation needs help then use those toe extensors (extensors back transfer) to boost their power and go brace free (if old enough).
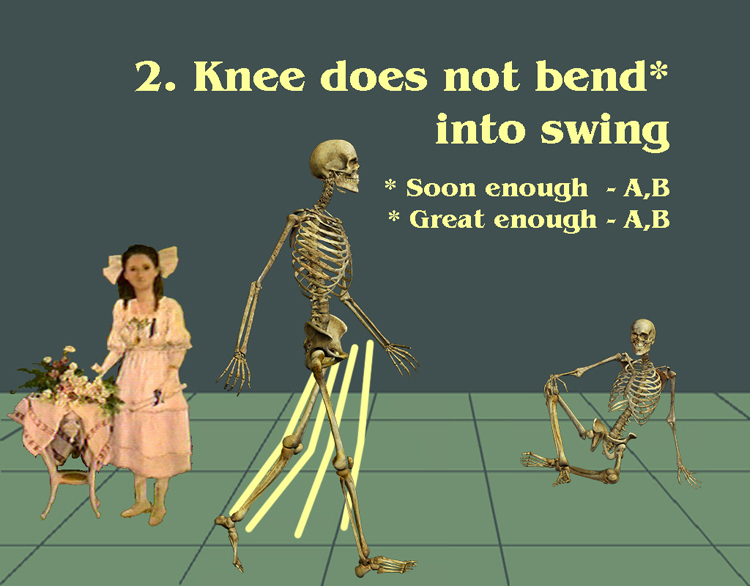
Group two. The big disability in hemiplegia is failure to bend the knee in swing phase. It is destabilizing in its requirements and an energy killer. It is NOT enough to bend in swing, it has to bend quickly without delay. I swear, if I see one more gait analysis that looks at swing RANGE of motion without regard to WHEN it initiates I'll . .I'll .. I'll write this. That's what brought this on. OK. I feel better now. We are in group two so we know the knee isn't bending enough soon enough. But WHY?
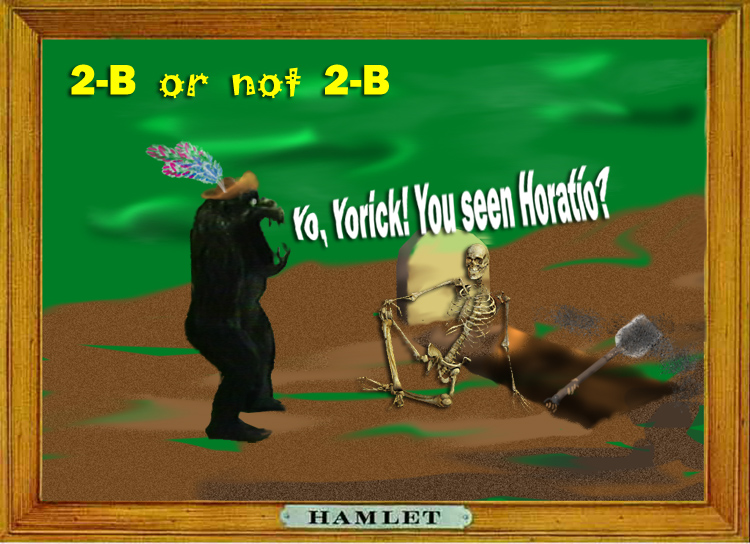
Yorick know of what he speaks. The knee may be held in extension by muscles that extend the knee. That's group 2-a. So group 2-a is when faulty neuromuscular signals make the knee ACTIVELY extend. But group 2-B is reactive. Something mechanical is retarding knee flexion. That foot thing? If in equinus (foot stiffly downward) and the foot does come to the floor, it can drive the shin and thus the knee back. The knee locks up like a baby carriage lid lock. With the knee thrust back, it can't bend at all unless it is first unweighted. You have to shift body weight to the other foot to then begin the swing knee flexion. The energy bus is long gone. By the way, if instead, there is no heel contact and the stiff side foot stays totally on toe, the back knee is avoided. The knee has to flex more to clear the vertical foot, but if that knee flexing ability is there then walking is BETTER on toe than ramming a knee to smithereens by forcing the foot flat. Yelling at an ankle does not make it dorsiflex (go up). So the toe walking stiff knee may well be in group 1. So what do we have?
So is the 2-B case ALL mechanical? If it is, then it is merely a job to fix the foot and replace this case in group 1! How can we know? See the SAWCH discussion for how.
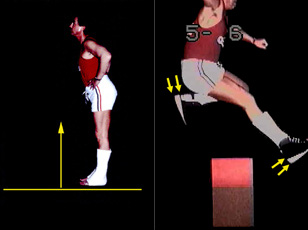
Putting wedges under the heel so that when the shoe bottom is flat to the floor the shin leans forward about 8 to 10 degrees (and the jackknife goes away) he then can walk normally and even run and clear hurdles. The double arrows point out the offset heel lifts that produce "FUNCTIONAL" dorsiflexion (a term used for stiff ankle conditions (AFO, cast, ankle fusion, ankle arthritis etc.).
So you attend to these foot details and it seems that the knee simply responds and bends in swing phase. This 2-B is what then?
That diploma, it's for using the whatsits. And THAT is telling us that to be is to THINK. So 2-B may well be a type 1. But 2-a, caused by knee extension muscles prefiring (too soon) and over firing (too long and too hard) needs consideration. Look at the image above. If the foot issues have been packaged in a mechanical solution, and a brief knee extension thrust happens here (as the hip hits full extension), then probably (OK, maybe) the stretch on the rectus femoris muscle that happens in this position is triggering a reflex to fire that muscle (or the quadriceps group). If THAT is so, then merely taking the upper end of the rectus femoris off the pelvic attachment (easy to do) will solve the problem. No yank - no yank back. Simple stop action video can usually sort this out. But be certain this is not what is happening in a dense hemiplegia.
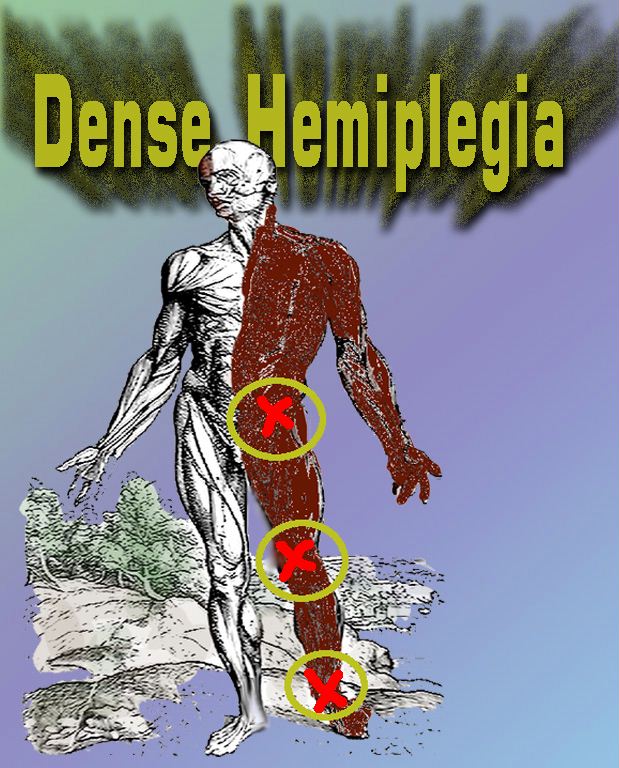
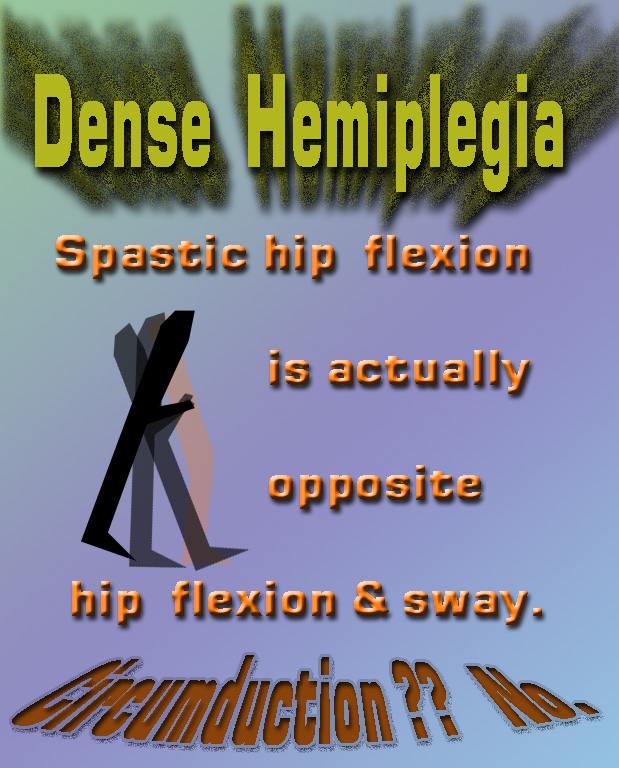
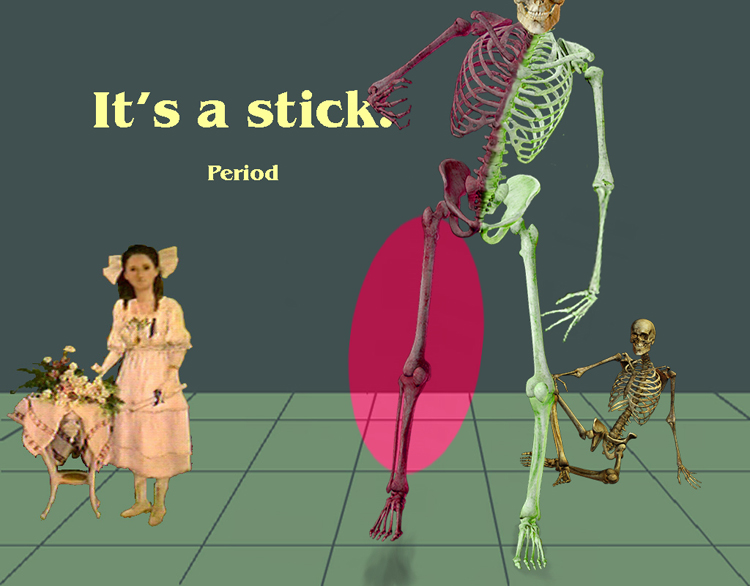
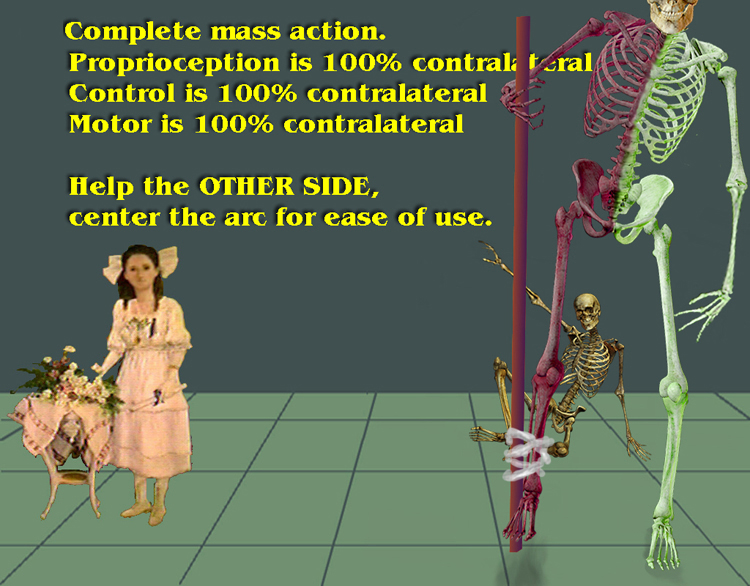
Dense hemiplegia has a wave of neurologic extension stimulus simply thrown at the leg. The joints lock up at all levels. The torso to foot is one long stiff stick.
What looks like motion forward and back on the stiff side is ALL coming from the uninjured side.
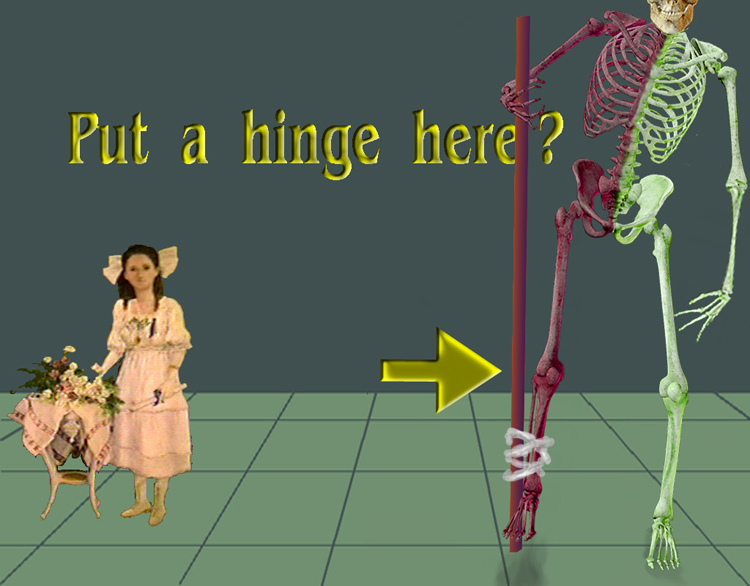
Beware! Dense hemiplegia has dense loss of sensory information and ability to quickly respond to change even if is is perceived. It is a mistake to make flexibility where there is no perception. If you broke your leg in the woods and used a big stick to get out, the singular nature of that stick allows it to extend perception. Knowing its length, when you place the stick you know where it is, securely. You can develop a bit of speed using that stick as a leg as the stick transmits its singular feel to your holding hands. Put a hinge in that stick and maybe some day they will find your bones in the undergrowth. So we don't want senseless bending of senseless legs. OK? But we don't want just any old stick. Let's use a good stick. A hockey stick? Handle end down. A stick that back thrusts every time you place it is a nuisance and energy killer. So a foot in equinus in dense hemiplegia isn't a good stick end. Really want the foot flat as the stick is vertical. Flexibility of the foot is irrelevant as long as the stick can roll forward.
Sensory loss can greatly mimic motor loss. Sensory deprivation causes the individual to just stay there. The hallmark is coaxing to just get started. They keep grabbing walls or objects or keep looking at the floor and their feet. Hemiplegias often have serious lack of knowing from the hand on top of stiff muscles. But there is another group, usually both sides of the body involved but not always (then they are called, wrongly, hemiplegia) whose main problem is sensory. The ataxias are in this group. That is another lecture. Dr. Yngve will be talking in detail about the stiff legged issues in great detail. So get a snack. Get that whatchamawhoozie fired up. There is another discussion of this same topic from another slant (that's what we do here, look from various angles).
|
||||||||||||||||||||||||
|
|
||||||||||||||||||||||||
|
|
||||||||||||||||||||||||
|
|


 The fellow in casts has the feet set in five degrees of equinus. Note the
locked knees and jackknife hip posture it takes to stand.
The fellow in casts has the feet set in five degrees of equinus. Note the
locked knees and jackknife hip posture it takes to stand. 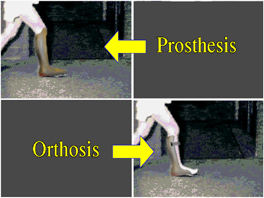 So stiff is stiff. A cast, a
prosthetic wooden ankle, an AFO made firm, a spastic foot held stiff - all the same. Even muscular dystrophy with all the calf muscle turned to stone, the same.
So stiff is stiff. A cast, a
prosthetic wooden ankle, an AFO made firm, a spastic foot held stiff - all the same. Even muscular dystrophy with all the calf muscle turned to stone, the same. The ^%$#$ hinge is NOT a hinge
if a stiff spastic foot is inside the AFO. The hinge does not allow any more motion. Indeed often makes for less. How? You've seen clonus. Allowing that upper thrust at the toe only triggers a
strong downward reflexive reaction. That reflex ALSO may generalize to the knee as an extension thrust! In our study at the RERC (Harvard/MIT lab) we
found half of the cases with hinge AFOs were worse for the hinge by this mechanism. The therapists just can't learn this. Gotta be a therapist gene. If
instead, the AFO is a yielding plastic, it shields the peak thrust and allows more dorsiflexion than a hinge.
The ^%$#$ hinge is NOT a hinge
if a stiff spastic foot is inside the AFO. The hinge does not allow any more motion. Indeed often makes for less. How? You've seen clonus. Allowing that upper thrust at the toe only triggers a
strong downward reflexive reaction. That reflex ALSO may generalize to the knee as an extension thrust! In our study at the RERC (Harvard/MIT lab) we
found half of the cases with hinge AFOs were worse for the hinge by this mechanism. The therapists just can't learn this. Gotta be a therapist gene. If
instead, the AFO is a yielding plastic, it shields the peak thrust and allows more dorsiflexion than a hinge.