|
Sensory Considerations
The many definitions of cerebral palsy virtually ignore what may well be the most important aspect. We all know that the
brain has many parts. Any part or combination of parts can be damaged, incompletely formed, or made to fail by chemistry defects.
It isn't just oversight nor linguistic foible. We are willing to admit to motor impairments (can't hide them) but not to deficits in knowing, assimilation
of information, or of formulation of planning.
Whoever uses such a label gets slammed by angry responses. Yet, the very key to rehabilitation is NOT in the motor system but in the sensory. Ignore this
and you don't stand a chance. So, put your anger away. It's ugly. Put your verbal baggage down and toss out any PT babble you have learned. If you want to know how to get through this stuff, then you have to know.
Knowing is hard.
By now you know how I detest CP definitions. You may also have noted a slighting of "diagnosis" in this context. Why? Because we are about rehabilitation.
Diagnosis puts forth one (arbitrary) feature of a disorder as a title. Boom - done. It names something wrong.
Rehabilitation requires knowing what is still intact. It works from inventory - inventory of what is available and how so.
 Picture this. You are told that there is no lumber. No nails. No cement. No shingles. Here is some food. It is going to get even colder than it is. See you in 4
months. Without shelter, is that the end of you? No. You take inventory and solve the problem. Picture this. You are told that there is no lumber. No nails. No cement. No shingles. Here is some food. It is going to get even colder than it is. See you in 4
months. Without shelter, is that the end of you? No. You take inventory and solve the problem.
 Well, to rehab we need inventory. We approach inventory in this way. Well, to rehab we need inventory. We approach inventory in this way.
What is working. Working does not means doing anything "good" or even useful at the
moment. It just means that it can do something and that the something can be turned on and off at will with control through the range that is left to it. It might not be good enough for what
it was supposed to do, but maybe it can be useful for something else.
Hey. Are there two things doing the same job? Can one be spared? Look for spare parts.
What is trying. Sometimes an intact function is totally
overpowered by the defect. An intact muscle crossing a fused (glued motionless) joint might be doing zero, but yet detected as trying to act. These are tougher. You have to get a sense of it.
But the trick to telling potential is not in what it does but in how quickly it attempts
to work. Lag time is a critical feature of uselessness. Something that responds hugely after long delay is useless. A weaker but quick response might be more useful.
What is reacting. These are the weeds in our garden. Careful.
In neurologic syndromes, muscles which have no direct control (and therefore of lower utility) may come to life via alternate neural pathways. Usually those are not so useful. We do not
want to lean on them too heavily in our planning.
Example? Know anybody with a stroke? One side of the mouth is paralyzed ?? Tell them a really funny but juicy joke, the more
naughty the better. Watch that paralysis laugh. The deep down bits of our brains which convey body language, social nuance, sex, in subtle gesture have their own circuits. They may be
spared. But they are not likely to be harnessed into higher levels of controlled voluntary movement. An arm that raises in reflex to a head being positioned is just that. It does not mean
that wanting the arm to raise will make it raise.
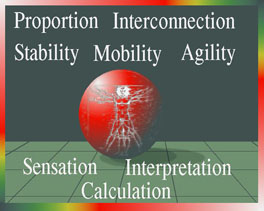 The devil is in the details. It takes much experience and knowledge to get it right. But, the ability to use some body part for a new manner of functioning
is totally reliant on sensibility. The devil is in the details. It takes much experience and knowledge to get it right. But, the ability to use some body part for a new manner of functioning
is totally reliant on sensibility.
Notice how it is even difficult to discuss. Words are lacking in the plain speak of conversation. Yet rehab-o-babble isn't much better. Weak side. Make it stronger. Pulling too hard. Trunk
weakness. Crouch. Firing out of phase. On and on and on... all about motor.
Weakness, weakness, strength, strength, weakness, strength, weakness, strength, weak, strong, .... blah blah blah... Hey, walls are strong and they don't walk.
The language is all about doing. What about knowing? Assimilating? Planning? Revising? Anticipating?
So how can you determine if a totally twisted kid has great potential for change?
This is important:
"The Moves"
Knock'em. How quick was the reaction? Not how good. How
fast? Instantaneous? With what? Something useful? Quick response means that there are intact sensibility mechanisms working with intact planning components. We call it "the moves".
You see a five year old struggling badly, hanging on a walker ineffectively, yet quickly responding to getting trapped,
stopping and resuming on queue.
We ask the older kids to point to a toe. Cover their eyes and you move their foot around and see if they can accurately point
at that toe regardless of where you position it. If they can track, then they can use that tracking information to new purposes.
Many of the walking disorders we see are sensory side. Yet time and energy is wasted on strength thinking. The youngster
zooms across the room with a walker looking like any kid who grabbed it for fun. Not leaning on it. Just holding it and zipping around. Then, placed in the middle of the room with nothing in
the hands - Boom. Hands go up, arms out, legs frozen. Urging gets only hesitant and small steps from stiff legs.
Why? Sensory. The youngster does not know what the feet are doing, where they are nor when. Spatial information required to
utilize coordination came from the walker through the hands. It wasn't "support", it was knowing, the wall you feel in the dark. Absent that, there is no secure way to make things move.
Let's look at some specifics and see how the knowing part is a better way to break down groups.
Hemiplegia:
Break this diagnosis in half twice.
1. Swing knee bend. The knee bends to allow the swinging leg
to swing. Seen in stop action, the knee flexes before the toe lifts from its planted place on the floor. Stated in another (better) way, the thigh swings without immediately displacing the
forefoot (thus initiating bending the knee). This timing is very fine tuned and relies on knowing. It implies knowing which in turn implies ability to adapt. On early hip flexion, the heel may well lift.
or
Not. Stiff knee preswing (and-or swing).
If not, is the knee prevented from bending by a stiff overplanted foot? ("ground reaction") A strongly down pushing
foot will, when planted, press the shin backward and block the knee from flexing into pre-swing.
So? That kills about 60% of the energy of gait, huge loss from a small brief defect. If you amputated the foot and put a rubber
fake in its place you would do far better, energy wise. You don't want to give up the knee to the foot. The knee is to gait what the queen is to chess. The foot is just a pawn.
Removing the foot: (mechanically)
So rethink, but with the foot removed from the experiment (which we call evaluation).
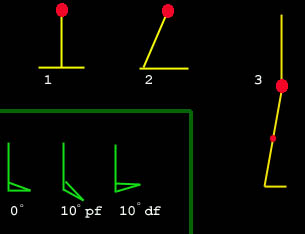 Put the foot in a cast
dorsiflexed 5 degrees or, if it is unable to get at least 5 degrees upward, then shim the heel (heel lifts) to make a similar angle. It is the angle between the bottom of the shoe (floor at mid-stance) and the shin. Put the foot in a cast
dorsiflexed 5 degrees or, if it is unable to get at least 5 degrees upward, then shim the heel (heel lifts) to make a similar angle. It is the angle between the bottom of the shoe (floor at mid-stance) and the shin.
Having made the foot  non-obstructive to the shin tilting forward, reassess the
knee without that pesky foot action. If the knee isn't under wrong control, it will now bend into preswing and replace this person into group #1 (if you can find a way to maintain what this
experimental cast is doing). non-obstructive to the shin tilting forward, reassess the
knee without that pesky foot action. If the knee isn't under wrong control, it will now bend into preswing and replace this person into group #1 (if you can find a way to maintain what this
experimental cast is doing).
Otherwise this person with hemiplegia is in group #2.
2. Knee does not bend in preswing.
If the knee does not bend in preswing, and it isn't an indirect defect (foot pressing shin backward) then ask why.
Rectus femoris?
One portion of the quadriceps muscle reaches upward, above the hip, to attach to the pelvis. It can be called upon - in times
of need - to add power to forceful hip flexion. When the walking hip extends, this one portion of the quadriceps gets elongated by way of this pelvic connection. It is wired to
quietly enjoy the ride - usually - and do nothing.
But, were it to react to (turn on) being so stretched, as the hip extends (end of stance phase, right before swing phase), then it
would contract at precisely the wrong point. Wrong? Why? Because the OTHER END extends the knee. The knee needs to be allowed to passively flex as the hip switches into flexion. It
is the THIGH which flexes in early swing. The lower leg is passive.
If the reason for stiffness of the knee in swing phase is that the rectus femoris is reacting to hip end stretch by reflex (self
stimulated) at the end of stance, then detaching it from the pelvis fixes the defect (easy).
However, it isn't always so easy. The rectus femoris may be getting the wrong signal as part of a broad brain call up signal to
all known hip flexors. Ahhh. The knowing part. If the fine control stuff is not working, "mass action" (deeper more primitive) mechanisms may get called upon to at least do something even if not the perfect thing.
Although the rectus femoris is a component of the quadriceps (front of thigh) muscle, it can be called on - under strong need -
to assist the hip flexors. That hip flexion ability is the programming leak. Hip flexion may be so broadly signaled that anything (and its buddies) than can hip flex is included in the
neurologic signal shotgun blast. Again, the knee gets stiff just as the hip is about to flex - worst time - but not by reaction from the foot below but by command from on high.
This is when the operation for stroke suggested by Dr. Jacqueline Perry at Ranchos Los Amigos gets its best usage.
The rectus femoris gets its far end (knee) attachment moved to the back of the knee so that it helps the knee bend rather than prevent it. No local fiddling with the muscle will turn it off.
Might just as well have it do the right thing.
But watch out. The patient MIGHT be better placed in group 3.
3.Entire involved side moves en bloc.
Just because the, say, left thigh is lifting forward, it doesn't always mean that the left hip is flexing.
Hmmm?
Visualize a fused - glued solid - hip. You could move that left knee forward at the end of a lifting thigh by LEANING BACKWARD from the other (right) hip.
Get that?
The well hip can extend to simulate the opposite stiff hip flexing. Here flexing really means moving the thigh forward,
because the stiff side does not really flex, the whole pelvis plus femur plus trunk lean, en masse, on the other hip (the well hip).
Again - the knowing. A dense totally diminished and stiff side does not KNOW. But, being densely stiff, it is like a board -
stiff as a board - or hey, how about a "peg". A peg leg works. Right? It is stiff. But it is also so stiff that it is reliable. It never
changes its properties. So like a sword being swung by a talented arm, a stiff half of a body can be swung by a talented other half of the body. What is working in this case of hemiplegia is the hemi not-plegia.
This is not merely a stiff knee. It is a stiff knee with a stiff hip.
Just more stiffness? Yes, that. But, more importantly when you see this, there is typically poor sensibility to the involved side.
They do surprisingly well even so. Why? Because there isn't anything to figure out. It all moves like a single board and the
motion is all coming from the good side. Like swinging a bat or fencing. The bat and foil do not need to feel. They are not doing the swinging. But imagine if the bat or the foil had a
hinge in the middle - and nothing to control that hinge. They would not be so precise in what they do.
So beware. Range of motion which is generated in a part that has poor sensibility will degrade performance. Sensibility is not
just the ability to feel something touching. It means the ability to sense movement, pressure, speed, acceleration, tension, and position in space. Sensibility is far more important than mobility.
 OK. OK. So? So, a plan that does not even consider the level of sensibility or somehow give it a once over is a crap shoot. OK. OK. So? So, a plan that does not even consider the level of sensibility or somehow give it a once over is a crap shoot.
In fact, sensory testing can totally predict outcomes (measured as usage rather than looks) in upper extremity surgery. We can consider the hand to
be primarily a sensory tool that can do things. Many amputees shun prosthetics because they interfere with sensation - knowing. The flip side is that rebuilding or reworking the hand
will do very little that is functional unless there is sensation to allow it to be used.
Hard, huh? Still not quite sure of this. Hmmm? Look at this example.
It is a movie.
Watch it several times. If your viewer allows, pause it.
There are two parts, kind of before and after. The before is a longer segment. The rest is brief. In this segment the first
part is painful to watch. You want to leap up and catch the youngster who seems to have no motor skills. She is really trying her best to walk, but all you see is arm waving and
short bursts of near toppeling.
If you try to describe this, do you call it weakness of hip flexors? Of trunk? Of thigh muscles?
Now play this next movie:
 |
Given crutches, her walking seems as if she has nearly nothing wrong and picked up a set of crutches and played
at using them.
What are our eyes telling us?
Well, first of all, notice the base of support. With crutches, the floor area which is her base is the bottom of a pyramid.
Her head is the top point. And also note that those arms which had been flailing are working perfectly. No arm problem here.
Feet alternate nicely orchestrated steps with no hesitation and with excellent trajectories.
Why? With the prospects of falling eliminated, excellent motor control - that's right, excellent motor control - can
now just show itself. The many actions needed to control movement for balance are no longer needed.
There are actually two huge differences. One, we mentioned and is obvious. The wide stable base eliminates
most control needs relative to balance.
The other, not obvious, is that the arms - by way of those crutches - are sensing - that is, feeling - the ground along
with any bodily accelerations or pitches and doing so in a very fine way.
The sensory loss behind the insecurity seen in the first video segment is made less consequential by utilizing an
inherently stable mechanism (what you would build into a wind up toy that just does a series of movements unable to sense and adapt to what is going on).
But it does much better. We see that she is actually getting the needed adaptive information by way of her hands. HANDS!!! Hands are magnificent sensory tools!!! Crutches do not just support - they feel - they tell, they probe change and allow smart control.
If you were in an unfamiliar dark room on a rolling ship, you just know that your hands would be out there groping
the walls and furniture for guidance.
AFO? Well if we make them too MOBILE we also make her need for information greater. A flexible AFO (solid, but
thin plastic) will yield to needed angles but press on shin skin this way and that way telling her information. If that skin is spared, making the AFO shorter - to feel good about
how short it is - ruins the ability of the AFO to inform by way of skin nudging as to what the foot to shin interaction is doing.
When discussing elegance in movement, if you are using words which based on strength or range of motion, the
chances are quite high that you just aren't getting it. Ask this question: Is the movement we are seeing in this limb while walking like or unlike the manner of movement it has
when doing something else sitting? A well coordinated tantrum with beautifully executed kicks and punches can give the clues we need.
 The Wheel
- a clue. The Wheel
- a clue.
In 'walking' (as opposed to stepping), energy transfers from one leg to the other are important and seemless. There is a point at which stance is
being transferred from one side to the other. Here we see the right stance leg deferring to the left. It does not wait for confirmation of security but assumes it. The right heel is
already off the ground before the left is fully planted. Therefore a transfer of energy in momentum is happening from the toe of
one side to the heel of the other. The feet look like they are on the perimeter of a big wheel. When sensory mechanisms are unsure, or the sequencing is not reliable, then the stance side
stays fully planted until the other side goes flat and weight is shifted. We see two flat planted feet.
The young girl above has a missing forefoot on the left. Yet her ortho-prosthetic serves so well as to allow normal everything.
She preserves the wheel. 'Knowing', that is, sensory or motor planning or adaptive skills are intact and thus energy sparing wheel like transfer of stance occurs.
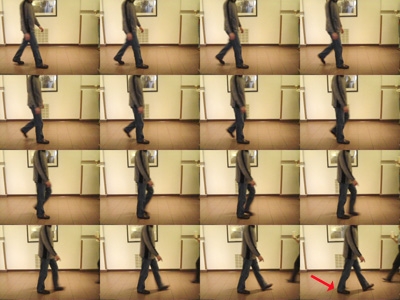 In contrast, the older male on the right, who lacks no anatomy, is brought by family members who say something
just isn't right about his walk. You get the sense of something subtle, but it is not something that jumps out at you. A shirt pocket digital camera set on multiburst makes the mechanical diagnosis. The wheel is
missing. Weight transfers occur late. That's why he is less inclined to like activities that require long walks (amusement parks). In contrast, the older male on the right, who lacks no anatomy, is brought by family members who say something
just isn't right about his walk. You get the sense of something subtle, but it is not something that jumps out at you. A shirt pocket digital camera set on multiburst makes the mechanical diagnosis. The wheel is
missing. Weight transfers occur late. That's why he is less inclined to like activities that require long walks (amusement parks).
 A small skin dimple near the tail bone gives away the rest. He is lacking some of the neurologic wiring that
does not much affect motor but which does rob him of subtle ground information. A small skin dimple near the tail bone gives away the rest. He is lacking some of the neurologic wiring that
does not much affect motor but which does rob him of subtle ground information.
When one leg has a knee go backward, recurvatum,
often the fear is that the knee will be wrecked. There is truth to that WHEN THE RECURVATUM IS ON THE WEIGHT ACCEPTING SIDE. When it is on the stance side, happening
late in stance, just before transferring to the other side, that is a sign of instability (athetosis, ataxia, sensory side disorders). It is
derived from leaving the foot flat - for security - until last moment and is happening in tension (which is not damaging).
Slamming the knee backward under weight landing is, on the other hand, the recurvatum we do worry about. That is recurvatum under compression.
 In an attempt to deal with sensory impairment we teamed up with some electrical
engineering folks in a frustrating series of near misses. Getting this right was not easy. Sensors in the shoes (getting the best trigger threshold for body weight can be maddening)
would trigger something worn on the chest to stimulate the skin on the chest. We mapped the chest to reflect the feet. Front=toe, back=heel, under arm pits = outer feet, near midline
chest = inner feet. Our devices also gave off red light as they stimulated so that we could track them visually on video. It was
very tricky to fine tune and consumed batteries to the point of being not so practical as we had to use existing pager parts, but it did work. In an attempt to deal with sensory impairment we teamed up with some electrical
engineering folks in a frustrating series of near misses. Getting this right was not easy. Sensors in the shoes (getting the best trigger threshold for body weight can be maddening)
would trigger something worn on the chest to stimulate the skin on the chest. We mapped the chest to reflect the feet. Front=toe, back=heel, under arm pits = outer feet, near midline
chest = inner feet. Our devices also gave off red light as they stimulated so that we could track them visually on video. It was
very tricky to fine tune and consumed batteries to the point of being not so practical as we had to use existing pager parts, but it did work.
In writing the section on SDR, it popped into mind that we
needed a similar easy term for apparent paralysis or frozen effort caused by the lack of knowing. A new term (use it please & spread it around): SDP.
Sensory Deprived Paralysis
I can hear them gasping already. But.. but .. paralysis is MOTOR. This is about language and diagnostic processing. It is also a darned good metaphor for what we are seeing - paralysis.
It supplies the mental linguistic link from paralysis, subtype sensory deprived, which right now nearly never happens and these kids go misdiagnosed often forever simply because the
current language lacks that logic branch.
The symptoms of SDP are a need to look at feet, strong need
for familiar place, and need for person to person contact if merely a shirt being lightly held
.
The signs, poorer skills in good braces, stance that maximizes
base including walkers kept far away, touching walls, following furniture, but more skill when pushing a weighted wheeled device. Does better barefooted even though feet look terrible.
Our use of minimal coverage spiral & floppy or flimsy braces are most suited to this group. Beware of this group and SDR as they may need the sensation more than spasticity reduction.
So back to those hemiplegia walkers. If the only problem is a stiff knee in preswing phase, but with good sense of self and
space, then we need to know what is making the knee stiff and get that out of the way. Given sensibility, the person with hemiplegia will do the rest. If it requires long intense rehab,
chances are that it was a case of low sensibility. Those with intact sensory will just know what to do. It may take some practice to tame it and refine it for changing circumstances and
crowded streets, but the underpinning is there.
There are two main things that impair the knee from bending just before the knee swings. Know this: the knee bend we are
talking about is passive. The thigh swings (hip flexes). The toe on the floor holds the toe as the thigh forward motion bends the
knee. As it lifts the knee the foot then passive swings out like a pendulum.
So, if the foot is too firmly planted with a stiffly down pressing ankle, then the knee can't bend. That is called ground reaction.
An easy diagnosis is had by applying a short cast holding the foot cocked upward by about ten degrees. If the foot was the impediment, then the knee should now bend for swing.
But if the knee is still very stiff, then active muscle action is at
work. The rectus femoris is the central slip of the quadriceps. It, alone of the four portions of the quadriceps, attaches above the
hip and can be called upon to boost hip flexion power. Consider it in the hip flexor reserves. In some cases of hemiplegia, all
potential hip flexors are fired off to start the hip flexing. That overkill broadness includes, then, the rectus femoris which will
stiffen the knee just as it is needed to be relaxed so that it can allow the knee to passively bend as the hip flexes. When this is
the cause, given reasonable other circumstances, then the knee end of the muscle can be moved to behind the knee where it will assist knee flexion rather than impede it.
In other sorts of neurologic conditions, the muscles are very stretch sensitive and may activate on being stretched. If the
rectus femoris is merely firing in response to being stretched by hip extension, then detaching the upper end will solve the problem. The is a much simpler procedure but requires that the
problem be specific reactivity and not "mass action". A sense of this can be gleaned from the manual exam. Although gait analysis can be useful here, we have seen many cases wherein
the interpretations far exceeded the data. Gait analysis is poor at testing sensibility. We can infer it from quality and speed of response, but we don't need computers to get that same
impression.
The hand is a big problem when a child ignores it. We see reports of improvement as ranges of motion and action on
command. Yet, as far as spontaneous use goes, nothing changes. What good is all this if it goes to naught? Doubling therapy - here defined as movement, strength, range, positioning and the
like - does not double anything of value. In fact little is anything may happen beyond the prevention of contracture.
However, spend time on sensory training with just the minimum range enforcement, and the hand becomes used more. This is
spontaneous usage, the only kind that really counts.
Get a cloth bag. In it place a Popsicle stick and an emery board. Have it examined (no peeking until after the feeling part) with
the good hand. Then repeat with the impaired side. The two sides will feel the objects differently. But we want to establish a kind of correspondence or equivalence. Then try a paper clip
with a safety pin, a nut with a bolt, a teaspoon with a soup spoon, a wooden letter N with a wooden letter M, a piece of burlap with a piece of satin, nickel with dime, dime with penny,
shoelace with electrical cord segment, and so forth. Do this every day as a game with rewards.
Some simply cannot learn this. The circuitry is just not there. But many can. Those that can do this get far more benefit than
having ten more degrees of thumb range.
In walking training, we must train the sensory mechanism. Paved roads and flat floors teach nothing. The legs must be
exposed to puzzles - changes in surface. Then the learning must figure what to do with that. Dirt is your friend. Use it. Bumpy surfaces with uneven slopes, broken sidewalks, odd surface
textures are where gait training ought to be. Nature is free. The facility pays rent by the square foot. Go outside!
The Hand
The hand gets special consideration because it is NOT a primary motor organ but more a primary sensory organ.
Meaning what? The function of the hand is far less driven by predisposed patterns of movement modified on the fly with
sensory feedback (as a second step fine tuning thing). In the hand, sensory information is right at the front line of function - doing anything.
This is the difference in walking (a basic leg function) with shoes and getting coins out of one's pocket (a basic hand
function) wearing gloves. It isn't the dexterity loss which so impairs as the discriminatory.
Functional results from hand surgery in the neurologic
conditions found lumped with CP correlate perfectly with sensory testing. Prosthetics fail terribly, regardless how magnificently constructed for detailed manipulation, when
sensation is not present and not provided. Amputees prefer sensate stumps more often than pretty but numb artificial limb ends for primary function (as apart from helper usage).
In a very real sense, our earliest goal is to know the future or at
least the possibilities. Measures of current skill do not lead us to such forward insight. However, getting a handle on sensory capacity does show us what is possible whether easy or hard to
procure.
|