|
Of all the chapters in this web site, writing this one is the most daunting. This web site is about savvy. Yet terminology required to discuss what is before us is seeping with old biases
and outmoded orientation.
Terms used for diagnosis are inevitably based on damage or fault or absence or something being amiss, one of whatever it is that we don't have. But from my perspective,
rehabilitation, our eyes should be on the lookout for what is still available to us.
 What can work or be made to work? We need INVENTORY. We have to work with what we have. So if you hear me going 'yeah yeah' about this diagnosis or that, it isn't that it lacks
importance but rather that it lacks the vantage point required to make it go away. What can work or be made to work? We need INVENTORY. We have to work with what we have. So if you hear me going 'yeah yeah' about this diagnosis or that, it isn't that it lacks
importance but rather that it lacks the vantage point required to make it go away.
So parents get angry if you inadvertently verbally equate CP with an anoxic event or a syndrome which caused bleeding and brain injury. But none
of those terms has any use to us. INVENTORY!
What does this individual have working?
What is trying to work?
What could be made to work?
What is the status of the control mechanisms?
Sensory mechanisms?
The last one listed is the most important of all because we are looking not for range of motion, but
control arcs. Control arcs are arcs of motion over which the patient has IMMEDIATE and fluid control. Control means that it can be started and stopped at will and by the person's own detection of need.
Don't mistake poor performance for poor motor skills. Often it is poor sensory input leading to absent
information with which to control motor skills. Please, if this is unclear, go to the sensory section.
Imagine the best car driver, ever, in a car with all the windows painted black. It is classic GIGO, garbage in garbage out, the car will crash.
Nearly all we do to rehabilitate draws on sensory integrity, yet none of the diagnoses even mention sensory deficit. You have to infer from the probabilities of what happened and how.
 Some kids react to sensation with poorly
controlled reflexic reaction. Having a "free ankle" will reflexly mess up the knee motion of many many spastic kids. Therapists refuse to believe that humans can't walk without free
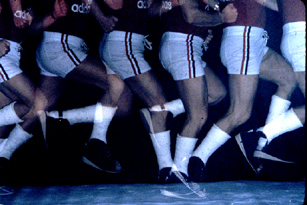
moving ankles (despite the fact that not a single amputee race has ever been won using an articulated ankle). Yet on the left is a subject wearing two casts set in slight equinus making
walking nearly impossible. By simply shimming the shoe and getting the shoe sole to tibia angle corrected (about 8 to 10 deg dorsiflexion), the subject can do everything including play basketball,
jump hurdles, and oh yes, walk. Some kids react to sensation with poorly
controlled reflexic reaction. Having a "free ankle" will reflexly mess up the knee motion of many many spastic kids. Therapists refuse to believe that humans can't walk without free
moving ankles (despite the fact that not a single amputee race has ever been won using an articulated ankle). Yet on the left is a subject wearing two casts set in slight equinus making
walking nearly impossible. By simply shimming the shoe and getting the shoe sole to tibia angle corrected (about 8 to 10 deg dorsiflexion), the subject can do everything including play basketball,
jump hurdles, and oh yes, walk.
If the foot is neurologically wired to make other things explode when the foot hits the ground, eliminate
the trigger. No hinge, but get the angle right, as above. Toes have to be supple to allow rolling forward.
But, if sensory input is poor, which means a reaction to motion is very unlikely, then shrouds around the
foot which further mask the outside world will make walking fail. Remove the brace or find a way to thin it to near minimum. Make the brace pliable so that the shifting brace ('sloppy brace') massaging
the calf and shin area increase tactile cues.
We even built a gizmo that senses pressures in the shoe and recreates them in a tactile way over the
chest (front of chest is toe, back of chest is heel, near sternum medial feet and below arm pits outer feet. It consumed too many batteries to be practical, but it did work. Careful, it does not produce walking.
It provides information which, given motor resources and computing capacity to use the information, can guide walking.
This is why so many kids walk near walls with a finger just touching or fleeting over furniture. They are
getting spatial information through the hands to offset what they are not getting from the feet. Often crutches are mere feelers just grazing the floor.
 Does the youngster really lean on
the crutch or is it a cuing tool? Parents ask when will mys child (who is getting about rather well in this way) be able to walk? The correct question is when will the person asking that question see
that the youngster IS walking. Does the youngster really lean on
the crutch or is it a cuing tool? Parents ask when will mys child (who is getting about rather well in this way) be able to walk? The correct question is when will the person asking that question see
that the youngster IS walking.
If progress is smoothly forward, of low energy, and without stoppages it is called walking. Above is a plot of distance versus time. If there are
hesitations, the graph forms steps. That is a stepper. If there is smooth forward motion the graph is a line whose slope is velocity of walking. This is the difference. Steppers use up all the energy in every
single step. Walkers conserve the energy by passing it from one step into the next. Momentum. Walkers have and use momentum. Steppers step. Walkers glide.
Would you like to feel like a stepper? Walk up stairs. Without momentum, we step. So 'walking' up
stairs is a misnomer? That is the problem with this topic. Our very words are tainted.
Brace strategies are different for steppers and walkers. Braces ought not impede the transitions (will
create a stepper). Steppers might need a bit of help at the transitions. A place to rest without using their own power.
Now we may see a kid turned at a strange angle to the direction of travel. Get out the chisel? Is he
WALKING? If it is >>walking<< that we are looking at, it could mean that the turned posture is a way of directing a more able mechanism toward the task of advancement.
Maybe that's where the controlled arcs reside. Be sure you don't redirect the part and in the process
direct the more usual but less able muscles to the task of advancement. Again, inventory. Is it a defect or a compensation? You may need to try a device that nudges this change you wish to see and
determine if function is maintained, bettered, or falls apart. When a good brace makes a kid worse there is huge information being given to you. Read the signs. Why did it fail?
The single most important finding when watching a kid with CP is to note how quickly the youngster
responds to an impediment or to something in the way or to being pushed or whatever. Not how well he succeeded, but how quickly he detected the need to do something. Fast response is very important.
It is a great measure of the sensory mechanism from input to processing for output. What the actual output does can be changed if we are clever. But our ship needs a captain and no fog.
Often a child "does well on the floor". On the floor, hard to pick out from other kids? That indicates that the tools we need are there.
Thick laborious movement does not do well walking. Walking needs rapid responses to perceived
changes. Thick overly stereotyped movement may do fine with stepping, but will not be able to chase the periodic reversals of the several pendulums involved in what we call walking.
There's more to life than walking!
Don't forget the spine.
Don't let nutrition slide when swallowing disorders make eating weird if not difficult. Please be on the
watch for the really skinny non-ambulatory kid. They are in serious danger. Their level of abnormal muscle tension is often amplified by the metabolic effects of malnutrition. If the kid is making tight fists
don't expect the stomach to just open gracefully to accept the needed volume required to be healthy.
A semi historical look at what we do:
In the mid 1860's Dr. Little made the observation that of the many sorts of deformity and infirmity seen
at that time, some were related to birth issues. He pointed out three main patterns of muscle stiffness: 1.
either the left or right side involved, or 2. the lower body involved, or 3. a generalized distribution. This very first formulation differs minimally from current ingrained terminology which refuses to elevate with
current knowledge. These conditions were called Little's Disease in honor of the author of these observations. Little had surgery performed on himself . It was designed by him, a Z shaped tendon cut.
He was a toe walker with tight Achilles tendons, though of what etiology is not clear. This was in the days before general anesthesia as we know it today, so ouch.
A very discerning and modern description of cerebral palsy was put forward approaching the turn of that century by the neurologist
we know of as the great psychologist Sigmund Freud. His amazingly detailed and correct descriptions would stand up to any recent critique.
After this, the literature becomes dominated by either the artful teachings of dedicated field surgeons (how to deal with this or that malady and how to evaluate needs of treatment based largely on
experience steered by study), or the more formal outcomes of strict laboratory experimental science. This has always been a dance of scorpions as the clinicians are suspicious of the relevance of
experiment made more pure than what exists in nature and also because the scientists are reflexly unable to admit that any fact is a fact unless put to a strict purified laboratory test.
Because multifactoral problems lend poorly to strict laboratory evaluation (it took Darwin trudging in
the field to get the big picture), the science has stood aloof from the practice and vice versa for a long time. More modern mathematical statistical methods have allowed a better interplay between medical
science and medical practice.
Things take time and many observers giving many supposed interpretations for the realities to sort out.
The physiology really came together when laboratory neurologic animal studies clicked in the mind of a traveling student, a future neurosurgeon (Peacock), who applied science which originated in a
physiology lab in Italy, and tweaked in France to children with cerebral palsy in South Africa. Parallel with that, better and more specifically targeted drugs with known actions have helped us know just
what was doing what and how. MRI has allowed us to actually see overt structural damage at an early time and distinguish structural damage from chemical abnormality. PET scans and functional MRI
methods are refining things even more. Old studies are being revisited with newer understandings in mind to better get at the applicability. The science has become awesome in applicaion in nurseries and
obstetrical methods.
The bottom line is that we are better able to sort out what is causing what and why. With that the
science can be better applied to actual cases and alternatives can be rationally discussed. It is way too big for anybody to do it all. We all try to contribute something, hopefully in areas where our own native
cognitive strengths are better served. Hopefully knowing why, we can prevent the problems.
Ahhhh prevention. Prevention is great. Yet three main patterns of muscle stiffness, persist 1) the left or
right side involved, or 2) the lower body involved, or 3) a generalized distribution as originally described by Little are still out there wanting better treatment choices. What has the science to offer as
to how to treat what could not be prevented?
First of all, we can simply accept the old diagnostic terms as being of historic interest and more
importantly of cost interest as they are what payers are using. It is VERY expensive to not use those terms, old and outmoded as they are. Until bureaucrats get their affairs in order we use those terms to
run cover for what we have to do. Obviously there are more than three kinds of problems in all of CP treatment. Obvious, huh? But not to them. So we accept the static encephalopathy or quadriplegia term
with a yeah, yeah. But treatment is to be based on the actual functional findings. Those go by systems and how those various systems behave.
[ ] Awareness of surroundings
[ ] Can decide what is wanted to do
[ ] Plans to do it reasonably
[ ] Does something within a reasonable interval from the perceived need
[ ] Does it directly
Completely if not perfectly
Incomplete, needs other assist as well
Uses alternative appropriate (clever) mechanism instead
Makes things worse
Knows it is worse
Unaware it is worse
[ ] Does additional things not constructive to the task
Spends effort trying to suppress the unintended extra actions
Can't weed out the extraneous stuff
[ ] Unrelated bodily postures in other parts make things change.
[ ] Regardless of how bad function looks, the part can move with minimal delay to a request to do so. That is, quick response to requests.
[ ] Performance visibly changes for the better when held or given tactile cues.
There are other things. We don't actually make printed check lists as the above would suggest, but
these are the things that the practiced eye is taking in. Of all of this, the best finding is ability of the youngster to make movements change quickly. Regardless of how poor the walking is, if crawling is
facile and with quick alternations of movement, then the chances are good that key control mechanisms are largely intact.
Why?
Well, function is about having intent and being able to act on it effectively - and safely. There are children who walk perfectly and do so right into walls and off precipices without apparent awareness of
consequences. That is a neurological statement. That kind of knowing resides in a particular part of the brain.
Parts of the brain govern intent. Other parts figure possible consequences. Other brain regions figure out motor sequences most appropriate to the current environment (motor planning) to avoid tripping or
to save energy or to aesthetically please an audience. Parts of the brain map kinds of motion and refine responses to get them better and faster and them assign those responses to other more automatic regions.
Parts of the brain measure how far the actual action was off from what was intended and then calculates a fix to improve it. The original sequence of movement, in fact, went out not as a stream of
signals to muscles but as a stream of intentions which get upgraded to two streams.
One stream, pyramidal, is a game plan of movement combinations (used many times before) with a degree of amplitude applied.
The second stream, (extra-pyramidal) which actually goes out slightly ahead is to all the input mechanisms to tell them what is expected to happen. What is coming.
When what happens is the same as what was expected to happen, the adjustments in the sensory mechanisms made by the forward signal stream result in no deviation detected and thus no need for
corrective input. When things don't match, the sensors send back data of the degree to which intent did not match the action. Much of the correction which follows is purely reflex at the spinal cord level.
many kinds and degrees of corrections reside in the spinal cord waiting to fine tune what we do.
When a person hurts their shoulder by lifting what was a heavy suitcase which somebody else emptied
secretly, the cause is exaggerated reflex response. It is not unlike pulling a finger quickly away from a hot object. The pull is well ahead of the ouch.
This fine tuning mechanism is initiated by sensory input and is a sensory mediated and big mechanism. It works from inherited predisposed movement schemes (inherited). Maybe some very practiced
movements get to this status as well, but higher up than the spinal cord. So we have brain areas that can append our automatic quick response list. The key feature of these kinds of movement is that they
are very stereotypical. A good model is the cat.
A cat has nearly no first stream. The cat moves by sending the data stream only to the anticipatory
centers which then reflexly produce the movements. Cats have a rich supply of such moves. Rich and finite. Cats are very adept at making a move perfect. The perfection is built into a single control loop
optimized for speed and agility. But not for novelty. It is old CATS that you can't teach new tricks. Nor young ones. Cats do cat stuff very well, but not much else. If cat sensory fibers are disrupted, they
become paralyzed. The sensory mechanism IS the motor mechanism.
We don't have such rich variation in a finite list of people moves. But we have the ability to keep adding
to he list. So hang gliding cats? No. Cats doing the Funky Broadway? Not in these parts.
Our key feature is versatility. Our biggest trick is the ability to conserve energy while traveling over
bumpy ground, of all sorts, on two limbs. We are so versatile, we can even generalize it to stilts, walking on hands etc.
So we are looking for versatility and efficiency if we are looking for function - people function. Both are tightly intertwined with sensory mechanisms.
Once we determine that the key features are intact, then we attend to the control arcs. Range of motion? No. Control arcs.
What's the difference? Range of motion is what range a joint can be put through, regardless of how long it takes or who is actually making it happen. A therapist? A control arc is the range which can be
quickly made to happen by the patient on request and how it is centered. You don't need much range to just walk on level ground. But the ranges of the many joints do have to be stacked, so to speak, so
as not to topple. Balance. Controlled balanced supple interactivity is a GOAL. Not so much range of motion, although range is nice.
Is there sufficient fast control to sustain momentum if upright (regardless of canes). If so go for the energy. Walking is a goal. Use of canes (for balance or feeling the floor) does not equate with not
walking. Smooth progression without stoppages is walking. If such control is lacking primarily in speed but not in form of movement, strive for stepping as a next best. But if bodily control allows no sense of
space nor anticipation skills, then assistive skills are sought - the ability to do pivot transfers etc. Just putting kids in wheel chairs because they can't walk or have no prospect to walk ignores the other
physiology we have learned. Weight bearing is needed to grow bone properly. Prolonged sitting causes severe joint contractures. One half of all the surgery I do is to undo the effects of prolonged sitting. We
ought not be filling out notes for how long a patient may be out of a chair but rather how long they ought to be allowed in them.
Healthy people having no medical issues have died of complications of single prolonged periods of sitting. Sitting is not benign. It is easy for care givers and appealing for risk aversion (lawyer fear) but
physiologically poor. So for those who must sit to function and be mobile, we need to structure sitting respites. Whatever can be done standing, do so. Use mat time as well.
The one sided case is a typical example of how a term poisons perception. Some of the diplegia children (PVL) have extension of the damage such that hands have some involvement (stroke has more
hand loss than leg). When such PVL has one side spared, we see kids being called hemiplegia and treated like stroke. That's no good.
In addition there are true hemiplegia subtypes which are quite distinct both in how they move and how
they can be made to move. To illustrate this, at a symposium, we offered a set of "identical quadruplets" (we made this up) who all had the diagnosis of right hemiplegia. Each had a different brain
cause with different findings and very different rehab approaches and surgeries. Though we never saw this happen, it is actually possible. How probable is to us and hopefully to you, not important. What is
unique to each child is important to that one child irrespective of the clouding terminologies and biases.
|